Causative & risk factors
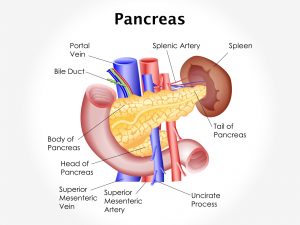
Gestational diabetes occurs during pregnancy, when the woman’s pancreas is unable to produce adequate insulin to stabilize the blood sugar levels. Being obese, having a family member with diabetes or belonging to certain ethnic groups are risk factors for developing gestational diabetes. Previous history of a stillbirth or giving birth to a baby over 9 pounds are other risk factors. Having polyhydramnios (excessive amniotic fluid) also puts you at risk of developing gestational diabetes.
Clinical presentation
Gestational diabetes does not produce any symptoms. It is diagnosed by a routine blood sugar test, typically performed once when pregnancy is detected and later between the 24th and 28th weeks of pregnancy.
Having gestational diabetes can harm the developing fetus. Gestational diabetes in the first trimester can lead to a birth defects and an increased risk of miscarriage. Gestational diabetes in the 2nd or 3rd trimester can lead to excessive growth of the baby, thus increasing the baby’s size. This can cause complications during labor and delivery.
Investigations
Gestational diabetes is suspected when blood sugar levels (fasting and post-prandial) are higher than normal. An oral glucose tolerance test helps to confirm gestational diabetes.
Treatment
A woman with gestational hypertension must monitor her blood sugar levels frequently to prevent damage to herself and her baby. Lifestyle modifications are usually sufficient to manage gestational diabetes.
- Diet – A low-calorie, low-fat diet is advised. Meal timings must be kept consistent. The patient is encouraged to eat smaller portions several times a day, rather than large portions at a time. Any food or drink that causes a sudden spike in the blood sugar levels is to be avoided. Examples of such foods include chips, sweetened drinks, desserts, deep-fried food and confectionaries. These are known as high glycemic index foods. Foods that increase the blood sugar levels steadily and slowly are recommended. Examples include whole grains, fruits, vegetables, low fat dairy etc. These are known as low glycemic index foods. One can enlist the help of a dietician to plan their meals.
- Exercise – The patient must determine a low to moderate intensity exercise plan with her doctor’s guidance.
- Weight management – Weight gain during pregnancy must be monitored by the physician since obesity increases the risk of developing type 2 diabetes.
If lifestyle changes by themselves are incapable of stabilizing blood sugar levels, the physician may prescribe oral anti-diabetic medications or injectible insulin.
Once the baby is delivered, the woman’s blood sugar levels usually return back to normal. However, women with gestational diabetes are at a higher risk of developing type 2 diabetes either immediately following delivery or in later life.



![Lobular Carcinoma In Situ [LCIS]](https://moho.loopshell.com/read/wp-content/uploads/2022/01/Lobular-Carcinoma-In-Situ-Lcis-300x300.png)