Causes and risk factors
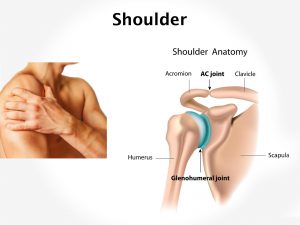
The exact etiology of frozen shoulder is not known. Advancing age and belonging to female gender make one more prone to developing a frozen shoulder. Other pre-disposing factors include rotator cuff lesion, trauma to the shoulder area, diabetes mellitus or thyroid disorders. Any condition causing relative immobility such as myocardial infarction, stroke or hemiplegia is associated with a higher risk of developing a frozen shoulder.
Clinical presentation
Frozen shoulder presents with progressive stiffness of the shoulder joint. Shoulder pain is initially present only at night, later at all times. There may be severe restriction of shoulder movements.
Diagnosis & Investigations
Patient history and physical exam is usually adequate to make a diagnosis of frozen shoulder. Sometimes your doctor may recommend an X-ray to rule out other pathologies of the shoulder. An MRI scan can show the inflammatory changes but is not routinely recommended.
Treatment
Frozen shoulder is a self-limiting disorder. Within 6 to 9 months, the pain subsides completely whereas the stiffness still persists. Medications and exercises help to bring back the shoulder’s range of motion.
Home treatment: Hot fomentation helps to relieve the stiffness at the shoulder. Physiotherapy is highly recommended to improve the range of motion.
Medication: Pain-relieving medications are prescribed. Hydrocortisone injections into the joint may be given.
Surgery: Manipulation of the shoulder under anesthesia may be attempted. Surgical removal of adhesions present in the shoulder may be considered if nothing else helps.