Causative and risk factors
The fungal organisms responsible for Athlete’s foot include Epidermophyton floccosum, Trichophyton rubrum or Trichophyton mentagrophyte. These organisms are collectively known as dermatophytes.
Athlete’s foot is a contagious disease and can spread from contact with an infected person or a contaminated surface. Anything that creates a warm or moist atmosphere in and around the feet can favor the growth of dermatophytes, thereby leading to Athlete’s foot. A few examples are:
- Wearing tight shoes, esp. for longer durations
- Wearing unclean/damp socks
- Wearing any kind of footwear that are too tight, or made of non-breathable material like plastic
- Walking bare-footed on moist surfaces esp. in communal areas
- Sharing communal bathrooms
- Sharing infected articles like towels, shoes etc
Clinical presentation
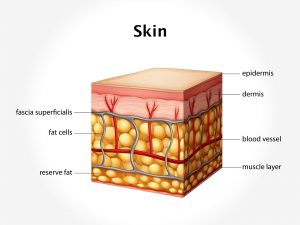
Athlete’s foot may occasionally remain asymptomatic. Usually, the patient develops a scaly red rash. It usually begins in the webs between your toes and later involves the entire foot. There is itching over the affected portion of the skin; it is usually worse at night. Dryness and peeling are present on the affected portion of the skin.
Athlete’s foot can spread to other parts of the foot and lead to Onychomycosis (infection of the nail bed), Tinea cruris (infection of the groin), Tinea corporis (infection of the skin over rest of the body), cellulitis, lymphangitis, lymphadenitis and secondary bacterial infections.
Diagnosis & Investigations
The diagnosis is based primarily on the skin appearance. If tests are performed, they may include culture, biopsy and KOH examination of the skin lesion.
Treatment
Several lifestyle changes are recommended in order to accelerate healing and prevent reinfection. Feet must always be kept dry. Wear cotton socks to absorb moisture and change them frequently. Wear breathable footwear. Avoid tight shoes especially for longer durations. Wear clean socks and change them frequently. Do not walk barefooted on any communal surfaces likes baths, poolside etc. Do not share towels or footwear with anyone.
Medication: Medicated powders containing anti-fungal drugs such as miconazole are to be applied to the feet. Medicated creams containg clotrimazole, ketokonazole etc are to be used on the affected areas. Oral antifungal drugs are useful in cases which are resistant to topical treatment.
In most cases, athlete’s foot responds well to antifungal treatment. However, sometimes fungal infections can be very difficult to treat. People with a low immunity and those living under compromised hygienic conditions may suffer from recurring fungal infections.
Recent updates
Studies are investigationg the efficacy of tea tree oil, vegetable oil, garlic and other natural treatments for athlete’s foot.