Causes and risk factors
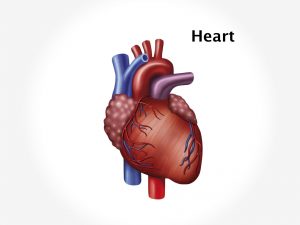
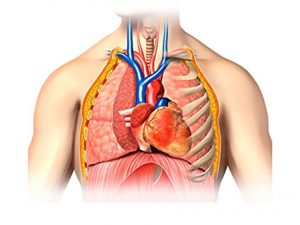
The exact cause of atrioventricular canal defect is unknown. It occurs when heart is developing during foetal growth. Atrioventricular canal defect can be partial or complete. In partial defect, there is a hole between atria [upper chambers of heart]. Also, there is defect in mitral valve [left atrioventricular valve] causing leakage of blood from left atrium to left ventricle [mitral regurgitation]. In a complete atrioventricular canal defect, there is a hole in centre of the heart affecting all four chambers which would normally be divided. There is a single common valve separating atria and ventricles [instead of two separate valves on left and right side of heart] which doesn’t close tightly. This causes mixing of oxygenated and deoxygenated blood. Thus causing more blood to flow to the lungs which increases work load on heart. Several factors may increase the risk of this congenital heart defect, such as Down’s syndrome in the baby, Rubella or another viral illness during early pregnancy, family history of congenital heart defect, drinking alcohol during pregnancy, poorly controlled diabetes during pregnancy, and certain medications during pregnancy. Atrioventricular septal defect may be associated with other congenital heart defects such as Double outlet right ventricle, single ventricle, transposition of the great vessels, Tetralogy of Fallot.
Clinical presentation
The child with AVSD has laboured feeding, tires easily, has shortness of breath, has heavy or rapid breathing, cyanosis, and frequent pneumonia. Child has poor appetite and no weight gain. Murmur is heard on auscultation of chest. Complete AVSD allows shunting of blood from one ventricle to the other. When it allows shunting of blood from left to right ventricle i.e. oxygenated blood mixes with deoxygenated blood and is transported to lungs. It increases pulmonary blood flow causing lung congestion and symptoms of pulmonary hypertension such as cough, dyspnoea, chest pain leading to congestive cardiac failure. Symptoms of CCF include fatigue, wheezing, excessive sweating, swelling in the legs, sudden weight gain from fluid retention, decreased consciousness.
Investigation
Medical history by the patient’s parents and Clinical examination by the doctor helps in diagnosis. A cardiac murmur can be easily heard on a stethoscope on auscultation which will diagnose CHD. Electrocardiogram [ECG], echocardiogram is recommended. Imaging studies such as Chest x-ray, Magnetic resonance imaging [MRI] of the heart may be useful for further evaluation. Cardiac catheterization is also advised in some cases.
Treatment
Treatment involves only surgical correction of the defective heart. Surgery is needed to close the holes between the heart chambers, and build new tricuspid and mitral valves. The timing of the surgery depends on your child’s condition and the severity of the disease, but it can usually be done when the baby is about 3 months old. Correcting an Atrioventricular septal defect may require more than one surgery. Surgery should be done as early in the baby’s first year of life as possible, before irreversible lung damage occurs. Avoidance of physical exertion in children is advised. Medications that help are those which increase the heart contractions, reduce the cardiac load and pulmonary congestion and regularise heartbeats.
Recent updates
Researches have been made in surgical robotics and ultrasound guided intracardiac surgery and tissue engineering to stimulate the growth of new tissue to repair congenital defects.