Causes and risk factors
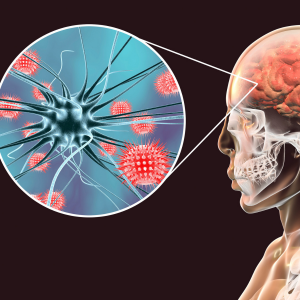
Various causes for coma are traumatic brain injury, stroke, brain tumours, hypoxia, exposure to toxins like carbon monoxide, lead and arsenic, drug and alcohol overdose. Metabolic disorders like diabetes, uraemia, hepatic encephalopathy, infections such as encephalitis and meningitis, seizures, systemic infection like septicaemia can also lead to coma.
Clinical presentation
Coma can be of various types such as Toxic metabolic encephalopathy which is reversible and caused due to illness or some systemic infection like diabetes. Anoxic brain injury due to lack of oxygen supply to brain. In Persistent vegetative state patient is in severe unconscious state and unaware of his surroundings; with breathing, circulation and sleep wake cycles; but no higher brain functions. Locked in state where whole body except eyes is paralysed, brain death i.e. irreversible stoppage of brain function. Medically induced coma i.e. anaesthesia during surgery or in acute severe brain trauma to control brain swelling. Signs and symptoms seen in a coma patient are altered physiological functions; irregular breathing, closed eyes or open eyes i.e. sleep wake cycle, lack of pupilary reaction to light, no movements, and no response to painful stimuli, light, sound with positive reflexes. Coma can be classified as reversible with residual symptoms and altered physical, psychological, musculoskeletal functions. Irreversible coma can remain for lifelong. Patient is prone to develop infections leading to septicaemia and death.
Investigation
Medical history by the patient’s relatives and Clinical examination by the doctor helps in diagnosis. During physical examination doctor will first elicit the reflexes, pupil reaction to light, response to pain stimuli, look for signs of trauma. ‘Glasgow’ coma scale is used for reference to detect the severity of coma. Blood test like CBC, BSL, serum electrolytes, thyroid function test, LFT is recommended. Lab tests to check for carbon monoxide poisoning, drug or alcohol overdose is done. Imaging studies such as CT, MRI scan of brain may be useful for further evaluation. EEG is advised in some cases.
Treatment
Treatment depends upon the underlying cause. Patient is treated in intensive care unit in initial period. First line of treatment consists of stabilising the patient by following basics ABC – airway, breathing, and circulation. Once the patient is stable, treatment will follow according to the cause of coma. Administration of glucose and antibiotics by intravenous route is recommended in case of hypoglycaemia or infection due to diabetes. Anti convulsants medicines are given in case of coma due to epilepsy. Surgery may be needed in case of injury to brain or brain tumours. Procedure is carried out to reduce brain swelling called craniotomy. They require full life support until the condition is reversed. Treating the underlying cause will contribute further to the treatment. Supportive care to prevent infections like pneumonia, bed sores is given. Physiotherapy to prevent contractures of muscles and deformities of bones and joints will also help in managing patients of coma. Adequate care is needed to maintain the nutritional status in a coma patient.
Other Modes of treatment
The other modes of treatment can also be effective in treating coma. Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating coma.
Recent updates
Therapeutic hypothermia [artificial cooling of the body] improve outcome of patients with severe head injury.
Facts and figures
Most comas end with eye opening and regaining consciousness. But 10% of those who open the eyes fail to regain consciousness. Patient over 40 years of age have poorer rate of recovery than younger patients. Absence of eye opening in first 30 days is indicative of poor prognosis.