Causative & risk factors
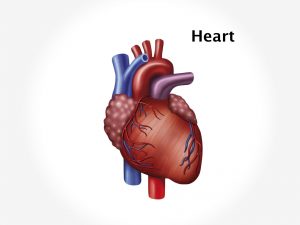
When Dressler’s syndrome occurs a few weeks after MI, it is believed to be immune-mediated. Certain antibodies are produced known as antiheart-antibodies which give rise to inflammation of the pleura and pericardium.
Similar symptoms can also be produced by trauma to the chest or after undergoing an open heart surgery.
Clinical presentation
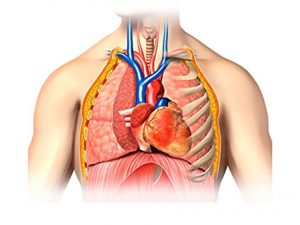
The classical symptoms are fever, pleuritic chest pain and pericarditis. Pericardial effusion may be present. Patient has a recent history of acute myocardial infarction. Pleurisy is produced which presents with pain in the chest. Pain may radiate to the left shoulder and is usually worse when the patient lies down. The patient experiences breathlessness with even mild activity. The fever is usually low-grade and is accompanied by malaise.
Dressler’s syndrome can result in complications like cardiac tamponade or pneumonitis.
Investigations
The patient’s medical history usually reveals a recent attack of myocardial infarction. On physical examination, the doctor can hear a pericardial rub.
Laboratory tests such as a complete blood count (leukocytosis), ESR (raised) and detection of heart antibodies in the blood are done.
An electrocardiogram and echocardiogram of the heart are performed. A chest X-ray is performed to note changes in the heart silhouette and surrounding structures. MRI scan of the chest is performed to view detailed images of the heart and pericardium and the lungs with the pleurae.
Treatment
Dressler’s syndrome is treated with aspirin, other anti-inflammatory drugs and steroids. Pericardiocentesis may be done to aspirate the pericardial fluid.
Recent updates
The incidence of Dressler’s syndrome has been found to be decreasing since it was first described.