Causative & risk factors
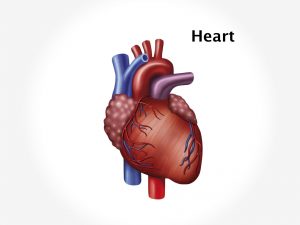
Endocarditis usually affects people who have underlying heart problems such as congenital defects or damaged or artificial heart valves. These conditions make the heart more prone to becoming infected with micro-organisms from other body sites. The common sources of infection include infected gums and teeth, skin infections and sexually transmitted diseases.
Dental procedures are a common cause of endocarditis. Contact with contaminated catheters, needles or syringes can also cause endocarditis.
Clinical presentation
Symptoms of endocarditis usually begin 10-14 days after the onset of infection. Non-specific symptoms like fever (with or without chills), malaise, night sweats and weight loss appear first.
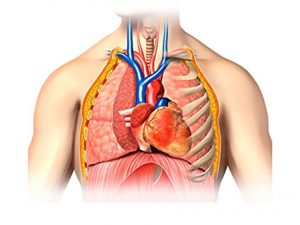
Tiny pin-point hemorrhages (petechiae) may appear under the skin and nails. Breathing becomes difficult and there is a persistent cough. Joint pains may be present. Osler’s nodes i.e. red, tender spots under the skin of fingers may be observed.
Endocarditis can give rise to several complications such as a heart attack, heart failure, stroke, heart abscesses and rhythm disorders of the heart.
Investigations
If endocarditis is suspected, blood cultures are done to detect the infective organism. An echocardiogram is performed to detect abnormalities or growths (vegetations) in the heart. A CT or MRI scan of the heart may be performed for a detailed picture. Other tests include a chest X-ray, ECG and urine examination. Cardiac catheterization is performed if necessary.
Treatment
Once the diagnosis is made, immediately intravenous antibiotic or antifungal therapy is started depending upon the infective organism.
If any complications develop as a result of endocarditis, heart surgery becomes essential.