Causative & risk factors
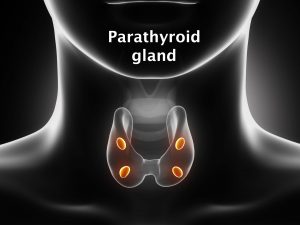
Depending upon the cause, hyperparathyroidism is classified as primary, secondary or tertiary.
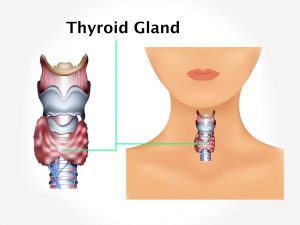
- Primary hyperparathyroidism: In this type, there is over production of parathyroid hormone due to enlargement of parathyroid glands, common in people >60 years of age and in women. Causes of primary hyperparathyroidism include adenoma on a gland, enlargement of parathyroid glands or a cancerous tumour.
- Secondary hyperparathyroidism: In this type, an underlying disease causes low levels of calcium in the body. Later the levels of parathyroid hormones become high. Causes of secondary hyperparathyroidism include severe calcium or vitamin D deficiency, chronic kidney failure and malabsorption.
- Tertiary hyperparathyroidism: In this type, even though the calcium levels have come to normal levels, the parathyroid gland keeps producing excessive parathyroid hormone. This is usually seen in people with chronic kidney failure, sometimes even after a kidney transplant.
Clinical presentation
The patient feels tired and fatigued all the time. His appetite reduces and he may have nausea and/or vomiting. The thirst and urination are both increased. The patient may complain of abdominal pain and is constipated. Calcium is lost from the bones leading to a loss of bone mass (osteopenia). Depressed mood is a frequent finding. In severe cases, the patient may become unconscious, develop high blood pressure or heart rhythm disturbances. Sometimes, the condition can even be fatal.
The complications of parathyroidism include damage to the kidney, kidney stones, peptic ulcers, pancreatitis and calcification of the cornea.
Investigations
The parathyroid hormone and calcium levels in the blood are high and the blood phosphate levels are found to be low. Secondary hyperparathyroidism can cause the blood calcium levels to become low. A 24 hour urinary calcium level will be measured.
Bone X-rays and a DEXA scan are performed to check the bone density. Ultrasound or CT scans of the neck are performed. A biopsy of the parathyroid gland may be suggested to rule out malignancy.
Treatment
On the basis of test results, if calcium levels are only slightly high, or if the bone density is normal, then the doctor will monitor your blood calcium levels twice a year.
Dietary changes will be recommended such as drinking plenty of water to reduce your risk of kidney stones and exercise regularly. The calcium and vitamin D which you get in your daily diet will be monitored.
Surgery: It is the most commonly used treatment; this involves removing enlarged parathyroid glands or tumours on the glands.
Secondary hyperparathyroidism: Here the treatment involves bringing the parathyroid hormone level back to normal, by treating the underlying cause. Doctor may prescribe vitamin D and calcium.
In some cases dialysis will be needed to treat chronic kidney failure.