Causes and risk factors
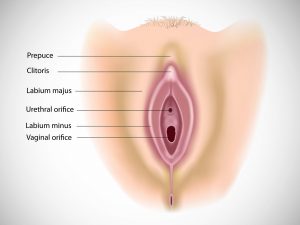
The exact cause of labial agglutination is not known. It may be a congenital abnormality. Labial agglutination may occur as a result of chronic vulvar inflammation from any cause.
Clinical presentation
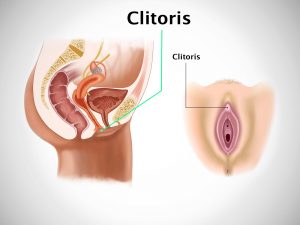
If the fusion is complete, it conceals the vaginal opening. If it is partial, it ends between posterior fourchette and clitoris. Mostly the patient is asymptomatic. Some clinical presentations can include urine pooling in vagina, post-urination dribbling. Patient experiences discomfort while urinating. Painful urination, altered urinary stream is experienced by the patient. There may be recurrent urinary tract infections.
Investigation
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Imaging studies such as x-ray pelvis, CT scan, MRI may be useful for further evaluation.
Treatment
No treatment is required for asymptomatic patients. Spontaneous resolution is common within 1 year or until the time hormonal changes take place when the girl reaches puberty. Administration of topical estrogen cream is useful. The area of agglutination [adhesion] will become thin as a result and separation can often be performed in the clinic with the use of a topical anesthetic. If this fails, further treatment may consist of surgical separation of labia.
Facts and figures
Estimated labial agglutination rate is 1.8% in girls between 13-23 months of age.



![Lobular Carcinoma In Situ [LCIS]](https://moho.loopshell.com/read/wp-content/uploads/2022/01/Lobular-Carcinoma-In-Situ-Lcis-300x300.png)