Causative & risk factors
The exact cause for the development of lichen planus is not yet known. It is believed to be an autoimmune disorder. The known triggers for lichen planus are certain types of medications, hepatitis C infection or a metal tooth filling. Certain forms of lichen planus tend to run in families.
Clinical presentation
Although no age group is immune to lichen planus, it is more commonly seen in middle-aged individuals. The symptoms of lichen planus are determined by which body part it affects.
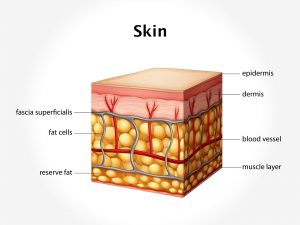
When the skin is affected, it produces several small bumps especially on the wrist, ankles or lower back. These bumps are reddish-purple in appearance and may have white lines across (Wickham’s striae). Itching may be present. The underlying skin usually becomes thick, scaly and rough.
When the mouth is affected, several tiny white dots appear inside the cheeks, on the gums, lips or tongue. The affected part of the mouth appears red and swollen and painful sores may develop.
Nails: Lichen planus can affect a few or all nails at a time. The affected nails become split and develop ridges and grooves.
Scalp affection is known as Lichen planopilaris. Tiny red bumps develop on the scalp. The hair may start thinning or falling off. Scarring takes place at the affected sites.
Investigations
Lichen planus can be diagnosed clinically by examining the skin, scalp, nails and the oral cavity.
When the diagnosis is in doubt, a biopsy of the affected tissue may be performed.
Treatment
There is no targeted therapy against lichen planus as it disappears on its own eventually. Treatment is aimed at bringing symptomatic relief to the patient.
Oral medications consist of antihistamines (to relieve itching) and corticosteroids (to reduce inflammation). Topical creams containing retinoids or corticosteroids may be prescribed. PUVA therapy is recommended to clear the skin.