Causes and risk factors
The common species include Rhizopus, Mucor, Cunninghamella, Apophysomyces, Absidia, Saksenaea, Rhizomucor, etc. The fungi are found in decaying organic matter, soil, leaves, compost pit, rotten wood, etc. Conditions that compromise the immunity of an individual are the main risk factors for developing mucormycosis, such as AIDS. Severe malnutrition can lead to the disease. Uncontrolled diabetes mellitus is the most common risk factor. Conditions like diabetic ketoacidosis, cancers, burns, medications that suppress immunity such as steroids and tumor necrosis factor (TNF) – alpha-blockers also increase the risk of infection.
Clinical presentation
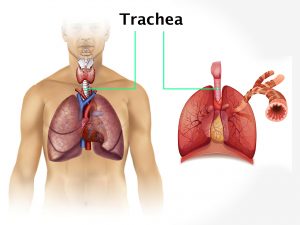
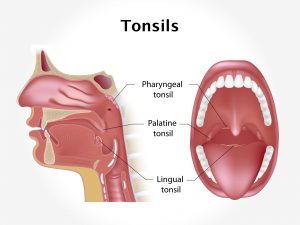
The commonly involved organs in mucormycosis are the sinuses, brain, and lungs. Other locations include the oral cavity, gastrointestinal tract, skin, maxilla, and other organ systems. The symptoms will vary according to the location involved. Rhinocerebral mucormycosis is characterized by the presence of reddish and swollen skin over nose and sinuses and dark scabbing in the nose. Additional symptoms include fever, headache, problems in vision, swelling of the eye, and facial pain. Pulmonary mucormycosis is characterized by the presence of cough with bloody or dark expectoration. Additional symptoms include fever and breathlessness. GI mucormycosis involves pain in abdomen, abdominal bloating and vomiting. Renal mucormycosis causes pain in the flanks and fever. Cutaneous mucormycosis can cause initially reddish and swollen skin often adjacent to an area of skin trauma that becomes an ulcer. Disseminated mucormycosis may initially begin with any of the above symptoms. Fever, headaches, and changes in mental status occur as the disease spreads to other organs.
Investigations
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Complete blood count usually demonstrates neutropenia. Biopsy of the affected tissue is done. CT/MRI scans if needed are done. CSF examination in cases with CNS involvement is required.
Treatment
Antifungal medications are helpful. Surgical debridement to remove all dead and infected tissue from the patient’s body is essential. At the same time, the underlying conditions such as diabetes, etc., must also be treated.
Complications
Complications such as disfigurement, blindness, meningitis, brain abscess, osteomyelitis, pulmonary hemorrhages, gastrointestinal hemorrhages, cavitary lesions in organs, secondary bacterial infections, or sepsis can occur.
When to Contact a Doctor
People with weakened immune systems must contact their doctor if they suffer from any of the above-mentioned symptoms.
Prevention
Avoiding contact with damp soil, compost pit prevents the disease. Immunocompromised patients must take precautions before going to such places. Wearing gloves, protective clothing while working in such places is necessary. Disinfection of cuts and scrapes after contact with soil thorough hand washing will prevent the infection.
Systems involved
Integumentary system, immune system
Organs involved
Skin, brain, respiratory system, central nervous system, GIT