Causes and risk factors
Erect posture, Lifting heavy weights, straining of pelvic muscles during vaginal delivery, obstetric trauma or frequent straining during defecation, chronic cough – bronchitis, weakening of muscles around vagina due to lack of oestrogen after menopause leads to rectocoele. Risk factors for rectocoele include genetics – born with weaker connective tissues, obesity, ageing – laxity of muscles.
Clinical presentation
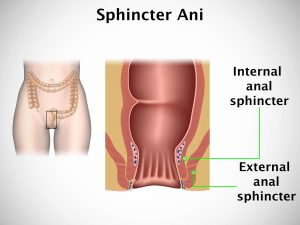
Patient presents with sensation of bulge in the vagina which might not protrude through vaginal opening, discomfort during defecation, constipation, and sensation of rectal pressure, incomplete defecation, and discomfort during intercourse. Many women experience other type of vaginal prolpase such as cystocoele or enterocoele along with rectocoele.
Investigation
Medical history by the patient and Clinical examination by the doctor helps in diagnosis. Pelvic examination which includes physical examination of vagina and rectum will help in diagnosis of rectocoele. Other investigations like x ray, MRI will help to further evaluate the disease.
Treatment
Asymptomatic rectocoele do not require any medical or surgical treatment. Doctor may advise diet involving high fibre food, drinking plenty fluids, lose weight in case patient is obese, avoidance of lifting heavy objects and straining during defecation, stool softeners, pelvic floor exercises, Use of pessaries [a device placed in vagina to hold bladder in place], hormone replacement therapy. Severe rectocoele require surgical correction or repair that will move rectum in place.
Other Modes of treatment
The other modes of treatment can also be effective in treating rectocoele. Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating rectocoele.