Causative and risk factors
Group A Streptococcus is also responsible for causing throat infections and skin infections. Scarlet fever can be acquired by coming in contact with or sharing things with other children infected by these bacteria.
Clinical presentation
Scarlet fever usually produces a fever of 101 F or higher with or without chills. Typical scarlet rashes appear as small, flat red patches which gradually become fine bumps and feel like ‘sandpaper’. They first appear on the neck, axillae and groin, and later spread over the entire body. Peeling of skin may occur as the rash passes away. ‘Pastia’s lines’ appear i.e. the skin creases of the underarm, elbow and groins become bright red, more so than the rash.
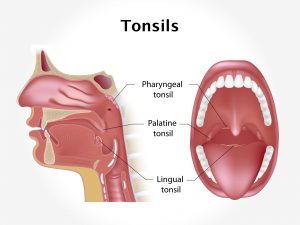
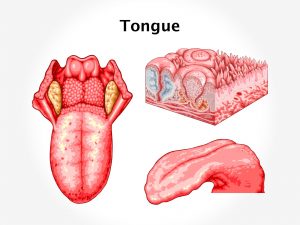
The patient has a flushed face and a reddish, bumpy tongue (strawberry tongue). There is inflammation of the throat and tonsils and enlarged lymph nodes in the neck. The patient may have a sore throat and difficulty in swallowing. Other symptoms include nausea, vomiting and pain in the abdomen.
Investigations
Scarlet fever can be diagnosed on the basis of the patient history and physical examination. Throat swab may be advised to test for Streptococcus A.
Treatment
Treatment includes a course of antibiotics. Other medications such as anti-pyretic drugs are given if necessary. The prognosis is excellent. Most children will recover even without treatment.
Sometimes scarlet fever can give rise to complications like rheumatic fever, glomerulonephritis, throat abscesses, otitis media, arthritis, pneumonia or skin infections.
Scarlatina can be prevented by following basic hygiene measures:
- Avoiding contact with an infected person
- Not sharing utensils with other children
- Washing hands thoroughly with soap