Causative & risk factors
Obstructive sleep apnea is caused as a result of relaxation of the muscles at the back of the throat. The airways get constricted, the blood oxygen levels drop and the patient is briefly awakened in order to breathe properly again. This cycle goes on repeating hundreds of time each night, thus preventing a restful sleep.
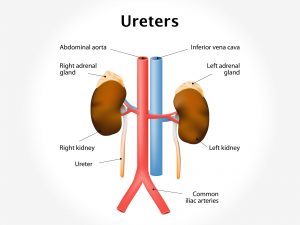
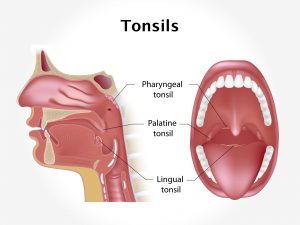
Obesity, advancing age, having enlarged tonsils or adenoids, nasal congestion or a thick neck are the risk factors for obstructive sleep apnea. The list also includes a family history of sleep apnea, advancing age and belonging to the black race. Intake of alcohol, sedative drugs or smoking can also predispose to obstructive sleep apnea.
Certain underlying diseases of the heart (heart failure, atrial fibrillation) or the brain (stroke, tumors) can give rise to central sleep apnea. Here the brain fails to give signals to the muscles of breathing and hence breathing stops repeatedly. The difference is that the patient is aware that he is being repeatedly roused and had difficulty falling asleep; whereas in obstructive sleep apnea the patient is not aware of being roused from sleep.
Both types of sleep apnea are more commonly found in males.
Clinical presentation
Patients with obstructive sleep apnea tend to snore loudly thus awaking their partners. On the other hand, patients with central sleep apnea are themselves awakened with breathlessness and choking sensation several times a night.
Since patients with sleep apnea cannot get restful sleep in the night, they usually feel very sleepy during daytime. They may suffer from insomnia and complain of headaches very frequently. They may have problems with memory and are unable to concentrate well. They frequently complain of a dry mouth or sore throat.
Sleep apnea creates a chronic deficiency of oxygen in the bloodstream and can give rise to several medical conditions such as heart disease, stroke, high blood pressure (hypertension) and depression.
Investigations
The patient’s sleep history is noted by questioning the patient himself and his/her partner. A sleep study (polysomnography) is carried out on patients suspected with sleep apnea. This machine monitors the heart, lung, brain functions, the blood oxygen levels and movements of extremities whilst the patient is asleep. Additional tests may include an electrocardiogram (ECG), electroencephalogram (EEG) or electromyogram (EMG).
Treatment
Simple lifestyle changes are advised initially which include losing excess weight, giving up smoking and alcohol and modifying the sleep position. Any underlying disease that may cause or contribute to sleep apnea is treated. If these measures don’t help, several devices are available to reduce sleep apnea.
CPAP (continuous positive airway pressure) is the most effective treatment for sleep apnea. Continuous oxygen is administered to the patient’s nose and mouth via a mask attached to a machine. If CPAP does not suit the patient, other devices are available which provide Bilevel positive airway pressure (BPAP) or Expiratory positive airway pressure (EPAP).
Your dentist can make specialized oral devices to reduce sleep apnea.
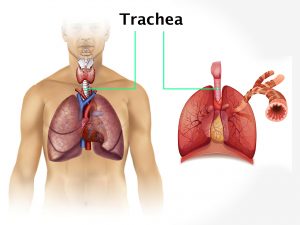
Once the above therapies have been tried without results for several months, surgery is the sole remaining option. Surgery may include removal of the tonsils, adenoids or nasal polyps; uvulopalatopharyngoplasty (removal of the structures at the back of the throat), repositioning of the jaw, tracheostomy (making an opening in the trachea and inserting a tube which has an open end outside the body) or insertion of implants.
Recent updates
A recent study demonstrated that sleep apnea remains undiagnosed in almost 40% patients with multiple sclerosis.
It has also been found that CPAP not only prevents further damage but can also reverse the brain damage caused by obstructive sleep apnea.
Nowadays, EPAP is preferable to CPAP because it is easier to administer and is more beneficial.