Causative & risk factors
Stevens-Johnson syndrome usually affects children and young people between the ages of 10 and 30 years. Females and HIV-infected persons are more commonly affected.
More than 3/4th patients develop this disorder as a result of certain medications. The most commonly identified drugs are sulfonamides, anti-virals, carbamezapine, allopurinol, anticonvulsants etc.
In the remaining 1/4th patients, Stevens-Johnson’s syndrome can be precipitated by certain infections or vaccinations.
Clinical presentation
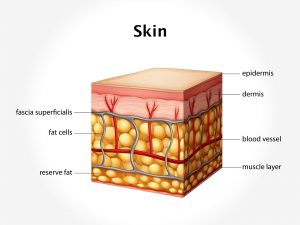
Stevens-Johnson syndrome produces hives, swelling of the face and tongue, skin rashes and peeling of the skin. There is blistering of the skin and mucus membranes. Involvement of specific mucus membranes will give rise to specific symptoms. The eyes may become swollen and pus-filled with scarring of the cornea. Affection of the urethra will make urination painful. Involvement of the rectum and anus will produce redness and burning in the perineum. Affection of the gastro-intestinal mucus membranes leads to diarrhea. Other symptoms include fever, weakness, soreness of the mouth and throat and coughing.
Severe or untreated patients of Steven-Johnson’s syndrome can develop complications like cellulitis, sepsis, skin disfigurement and damage to the internal organs.
Investigations
Steven-Johnson’s syndrome can be diagnosed on the basis of a medical history and physical examination. Sometimes a skin biopsy may be necessary.
Treatment
Steven-Johnson’s syndrome is a medical emergency and hospitalization becomes necessary for the patient.
If a medication is suspected to be the cause of this condition, it must be stopped immediately or replaced with a different drug. Intravenous fluids and nutritional support are provided to the patient. Painkillers, anti-histamines, antibiotics and other medications are given if necessary. A full recovery may take several weeks to months.