Causes and risk factors
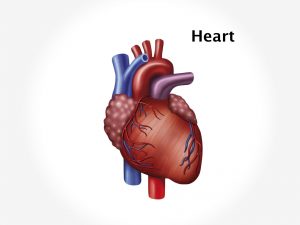
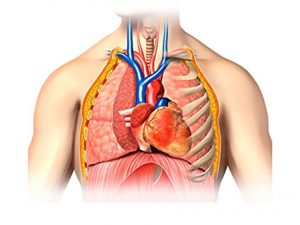
Exact cause of Tetralogy of fallot is not known. It occurs when heart is developing during foetal growth. The ventricular septum fails to form fully to separate right and left side of heart between lower chamber causing VSD. Pulmonary valve stenosis is a disorder involving defect in the pulmonary valve. It is either fused or thickened causing decreased blood flow form right ventricle to the pulmonary artery. Thickening of the musculature of right ventricle of heart is termed as right ventricular hypertrophy [RVH]. It develops in response to some factor which increases the workload on right ventricle causing the walls of the chamber to grow thicker; it loses its elasticity and eventually may fail to pump. Aorta is the main blood vessel which carries oxygenated blood from left ventricle to whole body. In Tetralogy of fallot, aorta is situated between left and right ventricles directly over VSD. Thus, deoxygenated blood flows from right ventricle to the aorta directly instead of pulmonary artery. Risk factors responsible for the deformity are age of mother [above 40], maternal nutrition, alcoholism, gestational diabetes, viral disease during pregnancy like rubella, family history of CHD or fallot’s Tetralogy and the newborn with genetic disorders like down’s syndrome.
Clinical presentation
Depending upon the severity of defect the Tetralogy of fallot shows various signs and symptoms such as with larger ventricular septal defect the child has symptoms like laboured feeding, tires easily, has shortness of breath, and has heavy or rapid breathing, poor appetite, and no weight gain. VSD allows shunting of blood from one ventricle to the other causing lung congestion and symptoms of pulmonary hypertension such as cough, dyspnoea, chest pain leading to congestive cardiac failure. Heart murmur, irritability, prolonged crying, palpitations, cyanosis are some of presenting features. Child may show Tet spells i.e. sudden cyanosis after feeding, kicking of limbs on waking, squatting to combat shortness of breath. Tet spells occur due to sudden fall in amount of oxygen in the blood. Baby is born with TOF are often referred to as ‘blue baby’ because of cyanotic spells.
Investigation
Medical history by the patient’s parents and Clinical examination of the child by the doctor helps in diagnosis. A cardiac murmur can be easily heard on a stethoscope on auscultation which will diagnose CHD. Pulse oximetry measures amount of oxygen% in the blood. A CBC, chest X ray, ECG is done. Echocardiography, cardiac catherization will confirm the diagnosis. A clinical test of giving supplemental oxygen does not alter the cyanotic spells in TOF in new born.
Treatment
Treatment Involves only surgical correction of the defective heart. Progressive hypoxemia and recurrent cyanotic spells indicate immediate surgery. It consists of intracardiac repair or a temporary procedure i.e. using a shunt between aorta and pulmonary artery. This increases the blood flow to the lungs. Post surgery, antibiotics to prevent any infections, avoidance of physical exertion in children, will also help in managing the patient.
Facts and figures
TOF affects 5 out of 10000 babies. It is responsible for approximately 10% of all congenital heart diseases.