Causes and risk factors
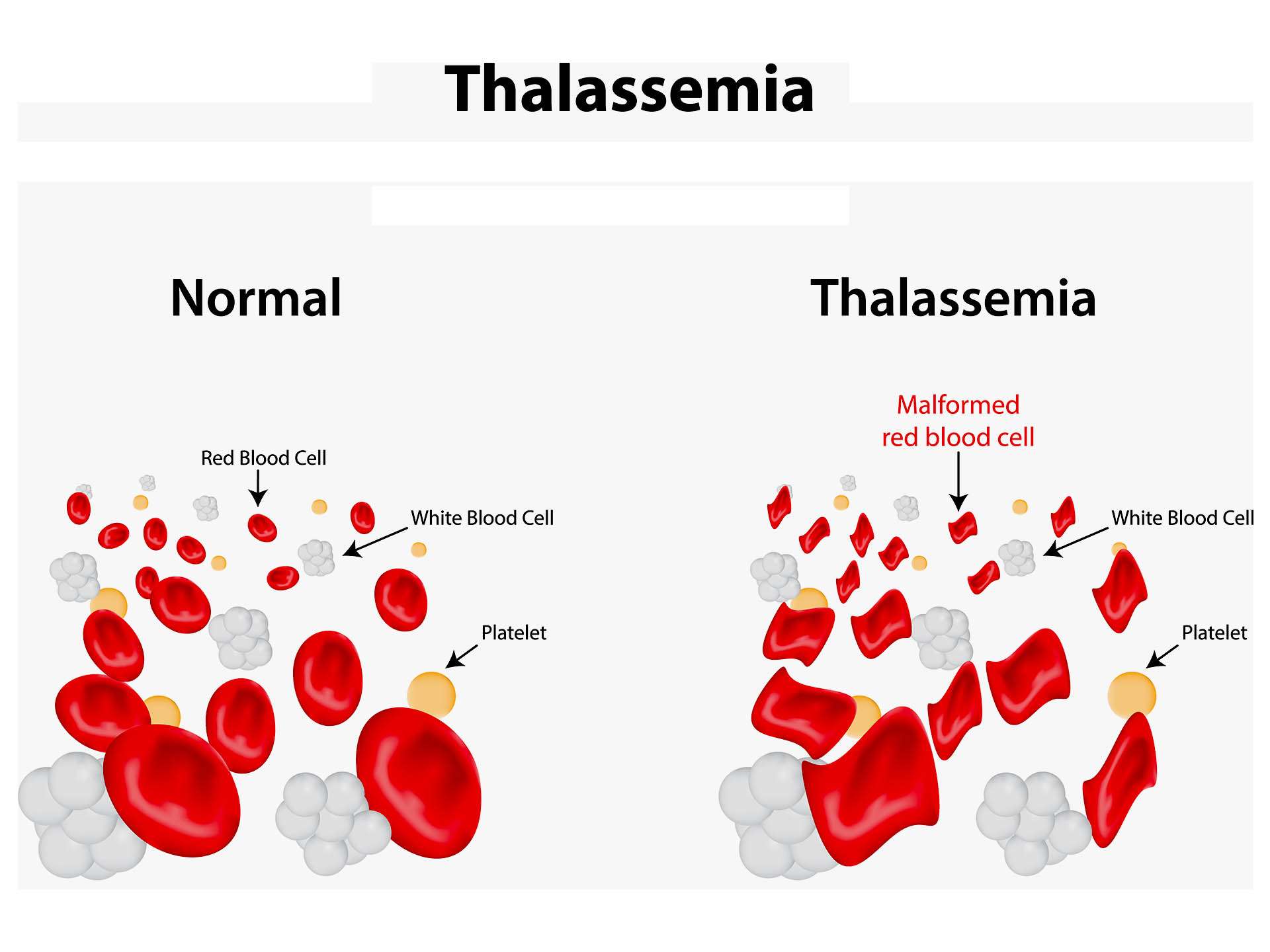
Thalassemia is an inherited disorder. Haemoglobin is made of 2 proteins – alpha and beta chains. Defect in the gene which is responsible for formation of these proteins leads to the disease. Alpha thalassemia occurs when there is defect in gene producing alpha globin whereas beta thalassemia occurs when there is defect in gene producing beta globin. Types of thalassemia are – thalassemia major and thalassemia minor. Thalassemia major is caused when the genes from both the parents are received. If genes are received from only one parent it causes thalassemia minor. In this the patient remains carrier of the disease and doesn’t show symptoms of the disease. The red blood cells are smaller in size.
Clinical presentation
Symptoms depend upon type of thalassemia. There are 2 types – minor and major in both traits alpha and beta. Alpha thalassemia is of various types – silent carrier state – in which the patient remains carrier of the disease and doesn’t show symptoms of the disease. Mild alpha thalassemia – lack of alpha globins is greater. The red blood cells are smaller in size. Patient shows signs of mild anaemia. Haemoglobin H disease – lack of alpha protein is great causing severe anaemia and signs such as enlarged spleen, bone deformities and fatigue. Haemoglobin H constant spring is more severe form with frequent enlarged spleen, and tendency to get viral infections. Hydrops foetalis or Alpha thalassemia major occurs when there are no alpha genes in child’s DNA which causes gamma globulin to form an abnormal haemoglobin called ‘haemoglobin barts’. It causes still birth [death of baby at delivery or during last stages of pregnancy]. Beta thalassemia has three varieties. Beta thalassemia minor is a carrier state in which the patient remains carrier of the disease and doesn’t show symptoms of the disease. Beta thalassemia intermedia in which lack of protein is greater; patient shows severe signs of anaemia. There are spleenomegaly and bone deformities. Children having beta thalassemia major is most severe form caused due to complete lack of beta protein. Children develop life threatening anaemia and require frequent blood transfusions. Associated symptoms include bone deformities in face, fatigue, failure in growth, shortness of breath, yellowness of skin and sclera [jaundice].
Inheritance pattern of thalassemia is as follows:-
When one of the parents is unaffected and the other is a carrier, there are 50% chances that the baby will be unaffected and 50% chances that the baby will be carrier. There are 0% chances that baby will get thalassemia. If both the parents are carrier, there are 25 % chances that baby will be unaffected, 50% chances that the baby will be carrier, and 25% chances of baby getting the disease. When one of the parents has thalassemia disease [thalassemia major] and the other parent is carrier, there are 50% chances of the baby being carrier and 50% chances of getting the disease. If both the parents are having thalassemia major then there are 100% chances of the baby getting disease.
Investigation
Medical history by the patient and Clinical examination by the doctor helps in diagnosis. A CBC is recommended which reveals anaemia. It will also reveal the size, shape, number of RBCs. A test called haemoglobin electrophoresis shows abnormalities in haemoglobin and is diagnostic of thalassemia. Tests before birth of the baby include amniocentesis, and chronic villus sampling.
Treatment
Treatment depends upon the type of thalassemia. No treatment is required for asymptomatic patients who are carrier of the disease. Mild thalassemia requires blood transfusions. Medical treatment includes folate supplements. Frequent blood transfusions are required in case of severe anaemia. Further treatment consists of stem cell transplant or bone marrow transplant which helps in treating the disease. Frequent blood transfusions can cause iron overload in the body. Chelation therapy may be required in such patients to remove extra iron from the body. Oral administration of iron supplements should be avoided in these patients. Prevention goes a long way to eradicate thalassemia. Antenatal maternal screening for thalassemia is recommended. Premarital counselling and avoidance of marriage between two thalassemia carriers must be avoided at all costs. The communities with high prevalence rate must be screened for thalassemia trait. School going child must undergo routine screening for anaemia and thalassemia trait screening for detection at early stage for further counselling. It is a social responsibility to prevent birth of a thalassemia child by proper antenatal surveillance.
Other Modes of treatment
The other modes of treatment can also be effective in treating thalassemia. Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating thalassemia.
Recent updates
Recently a new treatment called ‘gene therapy’ has been introduced at the annual meeting of American society of haematology. This therapy aims at reducing the number of frequent blood transfusions and increasing level of haemoglobin the blood.