Causative & risk factors
Normal working of insulin
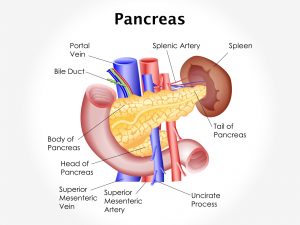
The beta cells (Islets of Langerhans) of the pancreas secrete the hormone insulin. Insulin is responsible for regulation of the blood sugar levels. Whenever food is consumed, the components of the food are broken down and the blood sugar levels rise. At such times, insulin is released into the bloodstream in order to facilitate the movement of this sugar into the body’s cells for energy. The amount of insulin released is in proportion to the blood sugar levels. Any excess sugar is converted into glycogen and stored into the liver, under the influence of insulin. During fasting or vigorous exercise, the blood sugar levels fall and so does the amount of insulin secreted by the pancreas.
What happens in Type 1 diabetes?
In Type 1 diabetes, the body is unable to produce insulin. Type 1 diabetes is an autoimmune condition, in which one’s own immune system attacks cells of the body. Anti insulin or anti-islet cell antibodies are produced and the beta cells of the pancreas are destroyed; thus producing absolute insulin deficiency. In such a scenario the blood sugar levels cannot be regulated unless insulin is administered from outside.
Clinical presentation
Diabetes is labeled as a ‘silent killer’. It is entirely possible to have diabetes for years and yet not notice anything abnormal. The classical symptoms produced by diabetes are polydipsia, polyuria and polyphagia. The person experiences a frequent need to urinate (polyuria). The person may need to have a lot of fluids to keep hydrated (polydipsia).The patient may feel very hungry even after intake of adequate food (polyphagia). This is because even though the person is eating; his cells are not being able to pick up the glucose from the blood. A person with type 1 diabetes may consistently lose weight. Since the cells are not getting enough glucose, the patient may feel fatigued all the time.
Long-term or uncontrolled diabetes can affect various body systems giving rise to a number of complications such as:
- Diabetic retinopathy – Uncontrolled blood sugar levels affect the small blood vessels of the eye giving rise to several eye conditions such as glaucoma, cataracts and even blindness.
- Diabetic nephropathy – Diabetes can affect the filtering units of the kidney giving rise to albuminuria.
- Diabetic ketoacidosis – The blood becomes acidic and there is accumulation of ketone bodies.
- Heart and circulatory disturbances – People with diabetes are at a higher risk of developing hypertension, stroke, ischemic heart disease and other conditions of the heart or blood vessels.
- Erectile dysfunction – Since diabetes affects the circulation, it can cause erectile dysfunction in men.
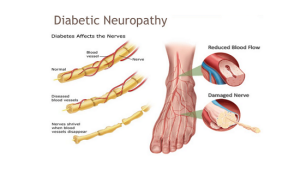
- Diabetic foot – Diabetics are prone to suffer from unnoticed foot injuries leading to formation of ulcers or gangrene.
- Infections – Diabetics have a higher susceptibility of catching infections compared to the normal population.
- Poor healing – Cuts, wounds, bruises or other injuries take a longer time to heal in patients with diabetes.
- Hyperosmolar Hyperglycemic Nonketotic Syndrome – This is an emergency condition characterized by very high blood sugar levels in the absence of ketones in the blood or urine.
- Peripheral arterial disease – Characterized by intermittent pain and tingling in the leg
- Diabetic coma
- Additional complications – Diabetic patients are more prone to hearing troubles and gum disease.
Investigations
Patients with type 1 diabetes will usually have a family history of a first degree relative with diabetes. The following tests are performed in all patients suspected with diabetes:
- Blood glucose levels – fasting, post-prandial and random levels are tested. Diabetes is suspected if:
- Fasting blood glucose levels, measured after at least 8 hours of fasting are higher than 126 mg/dL. The normal fasting blood sugar levels range from 80-110 mg/dL.
- Random or post-prandial blood glucose levels are higher than 200 mg/dL. Random samples are taken anytime whereas post-prandial samples are taken 2 hours after a main meal. The normal post-prandial blood sugar levels range from 110-140 mg/dL.
These tests can be easily performed with glucometers at home; however laboratory analysis using plasma yields more accurate results.
- Oral glucose tolerance test – The patient is instructed to fast for 8 hours following which, a measured dose of glucose water is fed to him/her. Blood sugar levels are tested before in the fasting state as well at several timed intervals after the liquid is fed. If the blood glucose levels are higher than the specified levels at the specified intervals on more than 1 occasion, the person is said to have diabetes.
- Glycosylated haemoglobin test (HbA1c) – These levels measure not just the current sugar levels but give an estimate of the average blood sugar levels during the past 1 to 3 months. Non-diabetic people have HbA1c levels of up to 6%. A reading of 6.5% or higher is suggestive of diabetes.
- Plasma fructosamine levels – Similar to HbA1c, this test also gives an estimate of blood sugar levels of the previous 1 to 3 weeks. Since the duration of measurement is shorter, this test gives a quick assessment of blood sugar levels over the past few days.
- Test for anti-Islet antibodies – This test is performed in children who are at a high risk for developing Type 1 diabetes.
- Urinary albumin levels – All pre-diabetic and diabetic patients must undergo testing for urinary albumin in order to detect changes of nephropathy.
Treatment
There is no permanent cure for diabetes. Treating diabetes is a life-long task. The aim of treatment is to stabilize blood sugar levels and prevent or delay complications. The treatment plan includes a combination of lifestyle changes and injectible insulin.
- Lifestyle changes: Lifestyle changes are essential for all diabetics, whether type 1 or type 2. The following changes are recommended:
- Diet – A low-calorie, low-fat diet is advised. Meal timings must be kept consistent. The patient is encouraged to eat smaller portions several times a day, rather than large portions at a time. Any food or drink that causes a sudden spike in the blood sugar levels is to be avoided. Examples of such foods include chips, sweetened drinks, desserts, deep-fried food and confectionaries. These are known as high hypoglycemic index foods. Foods that increase the blood sugar levels steadily and slowly are recommended. Examples include whole grains, fruits, vegetables, low fat dairy etc. These are known as low hypoglycemic index foods.
The American Diabetes Association, recommend that 50% to 60% of daily calories come from carbohydrates, 12% to 20% from protein, and no more than 30% from fat. One can enlist the help of a dietician to plan their meals.
- Exercise – An active lifestyle is recommended for all diabetics since a sedentary life increases the peripheral insulin resistance. Patients are advised to exercise at a moderate intensity 5 times a week.
- Weight management – It is very essential for a person with diabetes to maintain a healthy body weight, recommended for his/her gender, age and height. Obesity increases the peripheral insulin resistance, thus making it difficult to normalize blood sugar levels. Being obese as well as diabetic also puts you at a very high risk of developing heart disease.
- Insulin – Insulin is the primary line of treatment for patients with type 1 diabetes. Insulin can be derived from animals (bovine) or human sources. According to how quickly insulin acts, it is classified as rapid-acting, intermediate-acting and long-acting. Insulin is administered subcutaneously, either through pre-filled insulin pens or insulin pump.
Recent updates
Pancreas transplantation is a new and advanced treatment option. People with type 1 diabetes can receive a healthy pancreas from a donor. This procedure can cure diabetes and stop the need of receiving insulin; but it’s associated with several side-effects. Stem cell therapy is being tested in the hope of finding a cure for diabetes. Bariatic surgery is being considered as a supportive treatment option for obese diabetics. Newer tools and devices are being developed for the administration of insulin.