Causes and risk factors
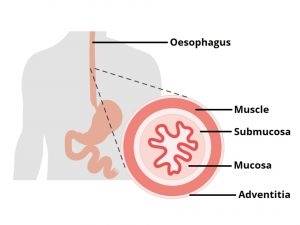
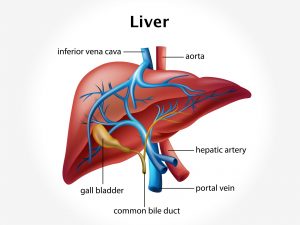
The most common cause of upper GI bleeding are peptic ulcer and esophagogastric varices. Additional causes include bleeding disorders, esophagitis, gastritis, erosive duodenitis, portal hypertension, malignancy, Mallory-Weiss tear. Some rare conditions such as angiodysplasia, hemobilia, pancreatic pseudocyst, Osler-Weber-Rendu syndrome can cause upper GI bleeding. Precipitating factors include use of aspirin, NSAIDs, anticoagulants, alcohol, etc. Other risk factors include people from lower socioeconomic class, chronic renal failure, etc.
Clinical presentation
Patient presents with abdominal pain, heartburn, dyspepsia, and dysphagia. Patient suffers from hematemesis. There is coffee brown color of vomitus. Fresh or brown colored blood is seen. There is melena, hematochezia, i.e., rectal bleeding. Pallor is seen. Rapid respiration is observed. Patient has a history of peptic ulcer, cirrhosis. History of prior bleeding may also be given. Weight loss, jaundice may be observed. Loss of blood can lead to shock, syncope.
Investigation
Medical history by the patient and clinical examination by the doctor helps in diagnosis. CBC, routine hemogram is advised. Hemoglobin level is estimated. PTT/INR is advised. Basic metabolic profile, BUN, coagulation profile is required. LFT is done. Globin level, gastrin levels are obtained. Endoscopy, chest radiography, and angiography is recommended.
Treatment
Bleeding should be stopped at first with the help of electrocoagulation, banding, or injection of vasoconstrictors at the site of bleeding. Oxygen supplement is given. After cessation of bleeding, gastric lavage is given. IV fluids are administered. Urine output is monitored. Further treatment depends upon the underlying cause. Coagulopathies must be treated with administration of FFP, vitamin K, cryoprecipitate, and platelets.
Facts and figures
Upper GI bleeding is a medical emergency and has 10% mortality rate.