Signs and symptoms
Commonest presenting features of jaundice are yellowish discolouration of skin and mucous membrane of the mouth and nose. Stool usually becomes pale in color and urine becomes dark coloured. It may be accompanied by itching. Some of the cases of jaundice may present with fever with chill, headache and body ache.
Pathology of jaundice
Jaundice is diagnosed by increased bilirubin level in blood known as hyperbilirubinemia. Bilirubin is a breakdown product of RBCs. Normal life span of a RBC is 120 days. Bilirubin is released during breakdown of ageing RBCs. Bilirubin is carried by blood to the liver. In the liver it is combined with bile. Thereafter it is excreted through urine and stool. Any disruption of this physiological process leads to jaundice.
Types of jaundice
Depending on the pathology, jaundice is classified into three types:
Pre-hepatic jaundice:
In pre-hepatic jaundice there is increased production of bilirubin due to increased breakdown of RBCs. Conditions that precipitate pre-hepatic jaundice are malaria, Gilbert’s syndrome, Crigler-Najjar syndrome, sickle cell anemia, thalassemia etc.
Intra-hepatic jaundice:
Intra-hepatic jaundice occurs due damage to the liver cells. As a result there is defective metabolism of bilirubin. Conditions that precipitate intra-hepatic jaundice are hepatitis, liver cancer, alcoholic liver disease etc.
Post hepatic jaundice:
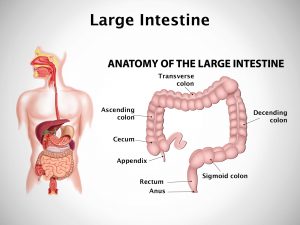
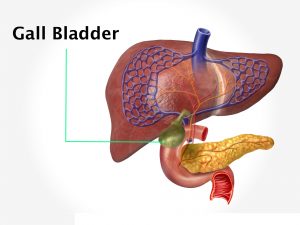
Post hepatic jaundice occurs due to defective excretion of bilirubin. Conditions that precipitate post-hepatic jaundice are gall stones, cancer of the pancreas and gall bladder. As a result excretion of bilirubin is obstructed. Post-hepatic jaundice is also known as obstructive jaundice.
Diagnosis
The physician makes provisional diagnosis by clinical evaluation. Clinical examination reveals yellowish discolouration of skin, mucous membranes of mouth and nose and sclera of the eye. Further questioning reveals excretion of dark coloured urine and pale coloured stool. Diagnosis is confirmed by estimation of liver function test. There is increased bilirubin level in blood. It may be accompanied by increased levels of liver enzymes – AST (SGOT) and ALT (SGPT). Alkaline phosphatise is increased in post-hepatic jaundice. In order to identify any underlying liver disorder USG and CT scan of the abdomen may be done. Tests may also be necessary as advised by the physician to rule out any other systemic diseases.
Treatment
Treatment of jaundice depends on the type, underlying pathology and severity of the jaundice. If any systemic disease is identified during evaluation, it should be treated accordingly. Apart from this treatment of jaundice is symptomatic and supportive. Drugs are prescribed for smooth bowel movement, prevention of gall stone formation due to biliary stasis, supplementation of essential nutrients and prevention of complications like hepatic encephalopathy.
Jaundice is a sign of an underlying disease. Underlying pathology should be evaluated carefully to cure jaundice.