Causes and risk factors
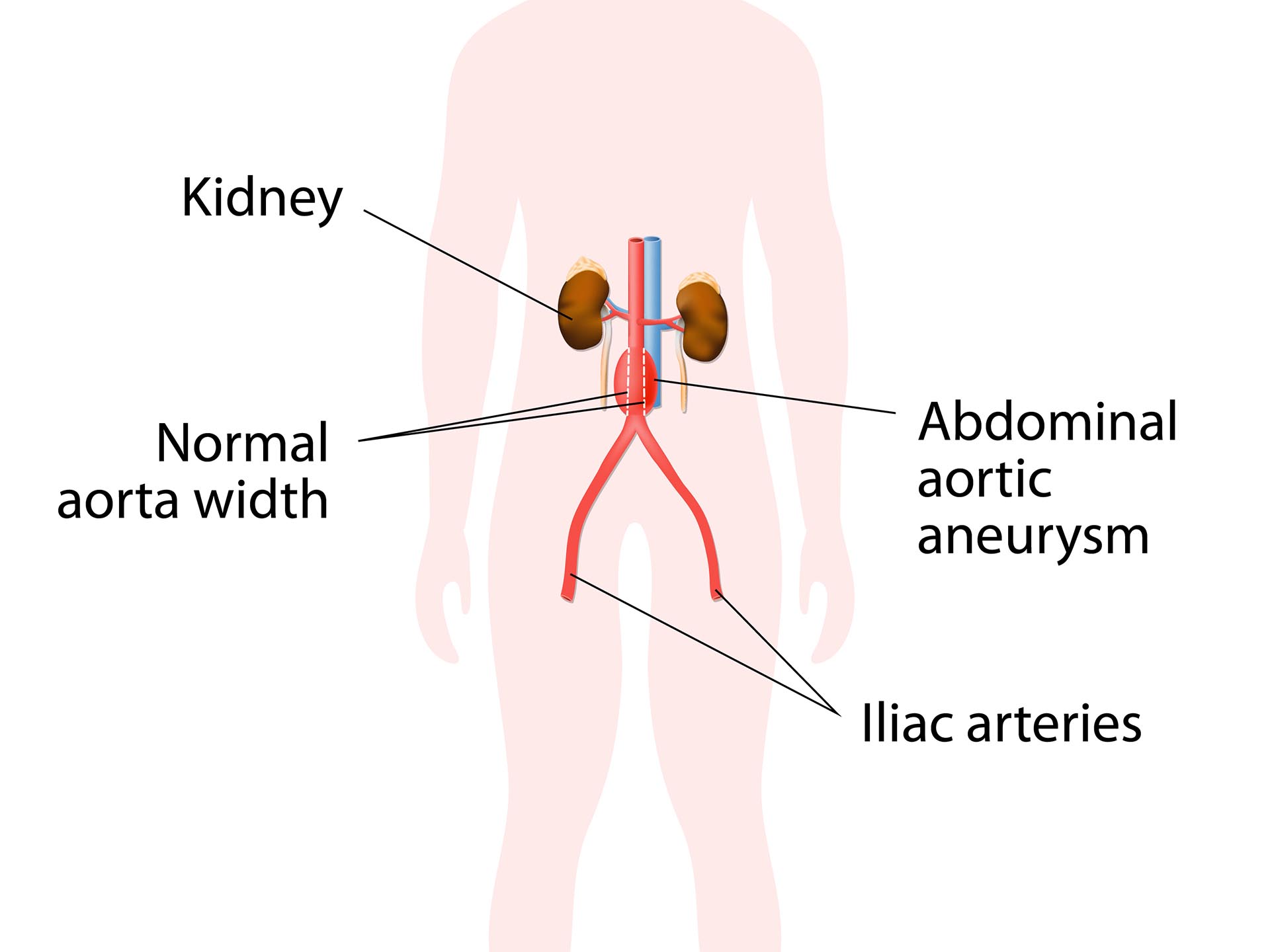
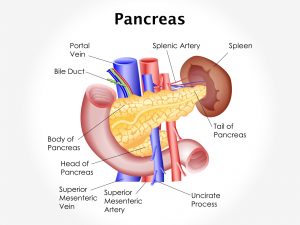
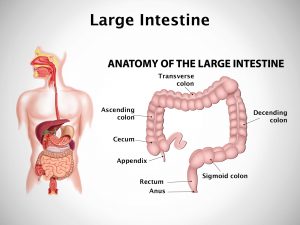
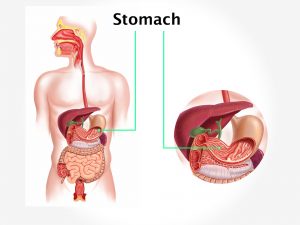
Various clinical conditions predispose to rise in intra-abdominal pressure and thus the syndrome. They are intra-abdominal or retroperitoneal hemorrhage, ascites. Gut edema can cause the disease. Intestinal obstruction can also lead to the disease. It can be caused by abdominal trauma. Risk factors include bowel distention in hypovolemic shock or due to massive volume replacement, ruptured abdomen, aortic aneurysm, acute pancreatitis.
Clinical presentation
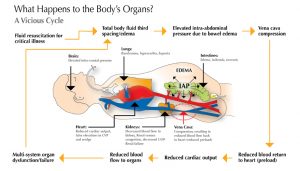
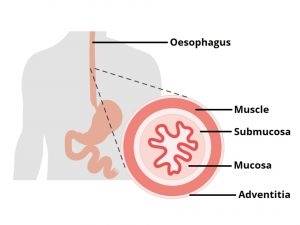
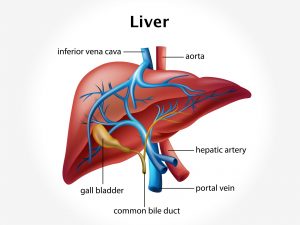
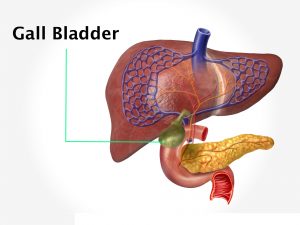
Several systems are involved in this syndrome. Increased abdominal pressure is transmitted to the pleural space causing reduction in lung compliance which leads to hypoxemia and hypercapnia. This leads to decrease in venous return, direct heart compression, and increased afterload. Reduced cardiac output causes reduced blood supply to the organs. Decreased perfusion to intra-abdominal organs can cause oliguria and renal failure. Decreased liver metabolism, splanchnic ischemia, bacterial translocation occurs. Reduction in perfusion of abdominal wall leads to impairment of wound healing. Intracranial pressure may be increased.
Investigation
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Intra-abdominal pressure can be estimated from measurement of bladder pressure. Alternative methods include indirect measurement of inferior vena cava pressure, gastric pressure, and rectal pressure. Abdominal CT scan is required. Comprehensive metabolic panel, CBC, lipase, and amylase levels are obtained. PT and PTT are estimated. Measurement of arterial blood gas is recommended. Urinalysis is done.
Treatment
Immediate treatment consists of shifting the patient to intensive care unit. Fluid resuscitation and transfusion is done. Open abdominal surgery may be useful in reducing intra-abdominal pressure (decompressive laparotomy). Laparoscopic drainage will also help in managing IAP. Continuous measurement of IAP is necessary.
Image – IAP