Causes and risk factors
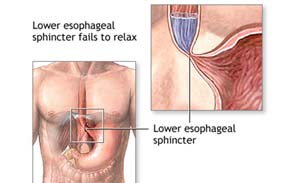
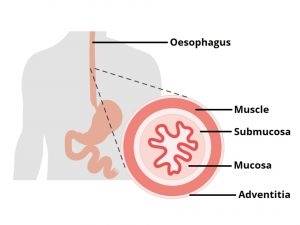
Achalasia may occur at any age, but is common in middle-aged or older adults. In achalasia, the lower sphincter fails to relax and open to let food pass into the stomach. The muscles of the lower half of the esophagus does not contract normally, i.e., peristaltic waves do not occur, thus, food is not propelled into the stomach. Factors causing achalasia are esophageal cancers, damage to the nerves of the esophagus, infection with a parasite, Chagas disease, and certain inherited factors.
Clinical presentation
Patient presents with difficulty in swallowing solids and liquids. There is regurgitation of food. Chest pain may be felt which is worse after a meal. The pain may radiate to arms, neck, and back. Patient complains of heartburn. Cough may be present. There is unintentional weight loss.
Investigation
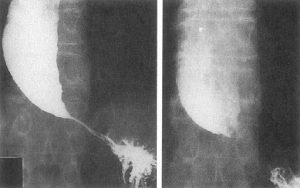
Medical history by the patient and clinical examination by the doctor helps in diagnosis. CBC is recommended. Esophageal manometry is done. Upper GI x-ray is advised. Upper GI endoscopy is done.
Treatment
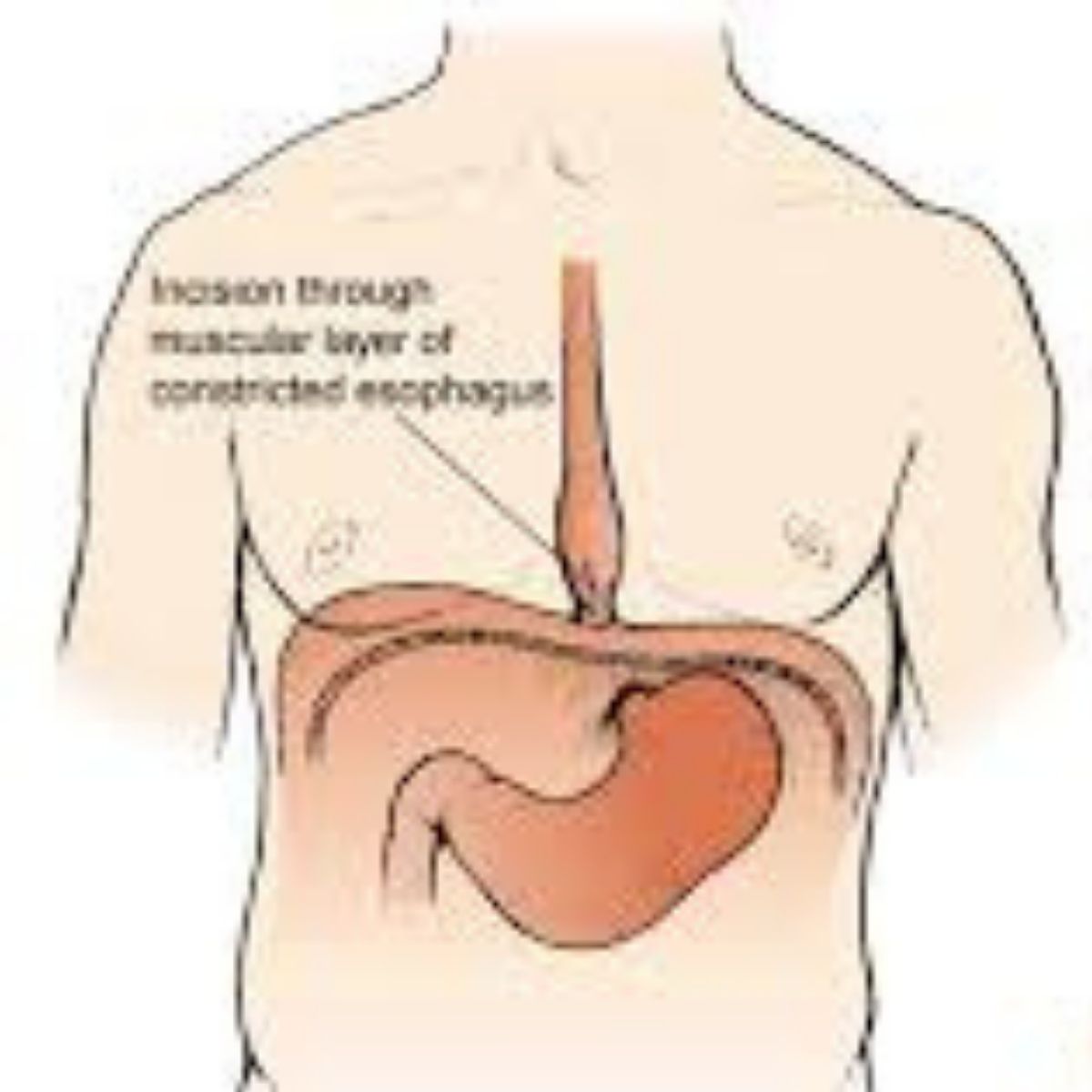
The aim of the treatment is to reduce the pressure at the lower esophageal sphincter. Dilatation – stretching of the lower esophageal sphincter is done. Oral medications can help to relax the lower esophageal sphincter. Botulinum toxin (Botox) is injected in the lower esophageal sphincter to paralyze it and prevent spasms. Esophagomyotomy surgery is performed to decrease the pressure in the lower sphincter.
Other Modes of treatment
The other modes of treatment can also be effective in treating achalasia. Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the Ayurvedic system of medicine, which uses herbal medicines and synthetic derivates, is also found to be effective in treating achalasia.