Causes and risk factors
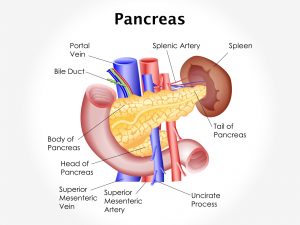
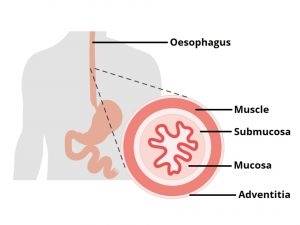
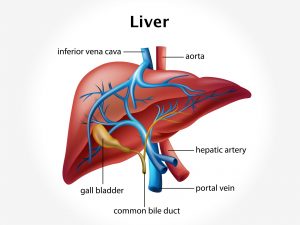
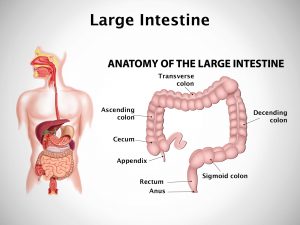
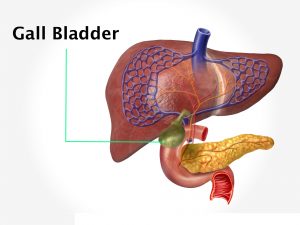
Amoebic liver abscess is a type of abscess in the liver caused by an intestinal parasite, Entamoeba Histolytica. The organism is carried by the blood from the intestines to the liver. E histolytica is present as two forms in the large bowel- identical-appearing cysts and motile trophozoites. In the absence of diarrhoea, trophozoites encyst in the large bowel. When the amoeba enters mesenteric venules, they enter portal circulation and reach the liver. The right lobe is affected more than left lobe. Transmission occurs through ingestion of cysts from fecally contaminated food or water. Flies and other arthropods also serve as mechanical vectors; transmission also results from contamination of food by the hands of food handlers. Where human excreta is used as fertilizer, it is often a source of food and water contamination. Person-to-person contact is also important in transmission of the disease; it can affect any one but the infection is more common in young and middle aged adults. Risk factors for severe amoebiasis include alcoholism, cancer, malnutrition, old age, pregnancy, recent travel to a tropical region, use of corticosteroid medication to suppress the immune system. Predisposing conditions for amoebiasis include crowding, poor sanitation, and poor nutrition. It is common in the age group of 20 to 45 years. It is 7 to 9 times common in males than females.
Clinical presentation
Person infected with E histolytica can remain asymptomatic or may produce signs and symptoms. It may take 2-4 weeks for the infection to manifest itself. Sign and symptoms of amoebic liver abscess include pain in abdomen, especially in right hypochondrium radiating to right shoulder, intense, continuous, or stabbing pain. It is accompanied by fever with chills, sweating. Features of jaundice are observed. Additional features include Joint pain, weight loss, loss of appetite, earthy complexion. Mild diarrhoea to severe dysentery occurs. Stools contain blood and mucus. There are stomach cramps, ulcerations in the colon can occur. Signs such as pallor, tenderness right hypochondrium, enlarged liver, intercostal tenderness, and basal Lung signs are seen. Extension of abscess to lungs or is a complication causing empyema or extension to abdominal cavity causing peritoneal perforation.
Investigation
Medical history by the patient and Clinical examination by the doctor helps in diagnosis. Tests include Complete blood count, Liver function tests, Serology for amoebiasis, Stool testing for amoebiasis. Imaging studies such as abdominal ultrasound, Abdominal CT scan or MRI, Liver scan is useful for further evaluation. Liver biopsy – rarely done due to high risk of complications. Aspiration cytology of the abscess is done.
Treatment
Medicines include antibiotics especially anti parasitic, antiprotozoals; anti spasmodic, NSAIDs. Fluid replacement therapy to replace the fluid loss is required by oral or intravenous fluid administration. Probiotics may be tried to help the growth of healthy bacteria. Surgical intervention is needed to drain the abscess. Prevention is possible by washing hands thoroughly with soap and hot running water for at least 10 seconds after using the toilet or changing a baby’s diaper, and before handling food. Cleaning bathrooms and toilets often; Avoiding sharing towels or face washers, avoiding raw vegetables when in endemic areas, as they may have been fertilized using human faeces, boiling water or treating it with iodine tablets.
Other Modes of treatment
The other modes of treatment can also be effective in treating amoebic liver abscess. Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating amoebic liver abscess.
Facts and figures
The infections are present worldwide but are most prevalent and severe in subtropical and tropical areas under conditions of crowding, poor sanitation, and poor nutrition. About 500 million persons worldwide are infected with entamoeba. Invasive E histolytica may constitute 5 million cases, with mortality in the range of 100,000 per year.