Causes and risk factors
The exact cause of aplasia cutis is not known. However, studies have shown that it is caused due to some mutation of gene which is responsible for the development of skin; however, which gene is involved is still not clear. Studies have thought that exposure to methimazole before birth causes this condition. Mothers who took these medications during birth increased their chances of giving birth to babies with these lesions. Viral infection during pregnancy and injury to baby during development are other predisposing causes. Aplasia cutis can be associated with certain other anomalies or malformations.
Clinical presentation:
Based on the number and location of lesion along with presence or absence of associated complaints, aplasia cutis is been classifies into 9 types: Type 1: In this a single lesion is seen on the scalp and there is no associated anomaly. Type 2: The lesion is seen on the scalp and limb; along with this, distal reduction of limb is seen. Type 3: Lesion is seen on the scalp along with epidermal sebaceous nevi. The patient suffers from complaints related to ophthalmic and nervous system. Type 4: The lesions are seen with hair color overlying deeper embryonic malformation. Type 5: the lesion is seen on the trunk and limb and is congenital, associated with placental infarct or fetus papyraceus.Type 6: Association with simplex, junctional, or dystrophic types of epidermolysis bullosa (EB) is seen. Type 7: Lesions are seen at the extremities without epidermolysis bullosa. Type 8: In this type, the lesions are caused due to teratogens. Type 9: In this, the lesions are associated with malformation syndrome. Areas with absence of skin are the characteristic features seen. It can be seen anywhere on the body. However, it is particularly seen on the scalp. The affected area appears like an open wound or an ulcer. The underlying tissues or even the bone can be seen. While in few cases these areas are healed. The shape of the affected area is either round, oval, or star shaped; the size and shape varies. In cases where this lesion is seen on the scalp, there is absence of hair growth on that patch. In certain severe cases where the underlying dura matter is also exposed, severe bleeding can occur. Exposure of the underlying tissues and bone increases the risk factor for secondary infection.
Investigations:
Diagnosis is done on the basis of the symptoms narrated by the parents along with clinical examination carried out by the doctor. Usually the examination of the lesion is sufficient for diagnosis. Investigations are advised to detect certain other associated conditions. It includes investigations like routine and specialized blood tests, CT scan, MRI etc. Histological examination of the lesion can be done.
Treatment:
In cases where the lesion is very small, usually they heal gradually. Local antiseptic bandages and topical applications are used to avoid infections and it aids in healing. Administration of antibiotic medication is the choice of treatment in cases if secondary infection supervenes. Large areas or areas which bleed need surgical treatment.
Complications:
Secondary infection of the exposed areas and arterial bleeding is a common complication seen.
When to contact a doctor:
If any skin lesion or wound like lesion is seen in newborn babies, one should immediately refer to the pediatric doctor.
Facts and figures:
Approximately 1 in 10,000 newborn babies suffer from this condition.
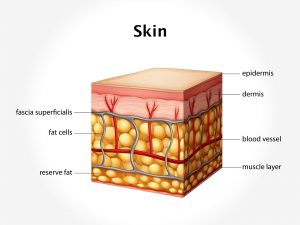
System involved: Integumentary system, genetic system.
Organ involved: Skin, bones, tissues and blood vessels, genes.