Causative & risk factors
Dermatomyositis is an autoimmune disorder wherein the body attacks its own cells.
Clinical presentation
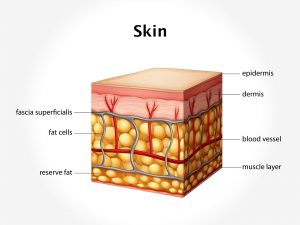
Dermatomyositis is characterized by changes in the skin and muscles.
Rashes appear on the skin of the face, elbows, knees, knuckles, back and chest. The rashes are purplish, bluish or dusky red in color. On the face, the rashes assume a butterfly shaped distribution affecting the eyelids, nose and the cheeks.
The muscular changes include stiffness, soreness and progressive weakening of several body muscles. The muscles of the trunk tend to be involved first followed by other muscles. The patient may find it difficult to perform day to day activities such as climbing stairs. The weakness goes on progressing and may involve the chest and esophageal muscles giving rise to difficulty in swallowing and breathing.
Calcium deposition can take place in the skin, connective tissues and muscles (calcinosis)
Having dermatomyositis increases your risk of developing other conditions such as Raynaud’s phenomenon, heart problems (myocarditis, arrhythmias, congestive heart failure), interstitial lung disease, certain forms of cancer and other connective tissue diseases.
Investigations
Blood tests are performed to test for presence of autoantibodies and to measure levels of creatine kinase (CPK, CPK-MB) and lactic dehydrogenase (LDH). Electromyography is performed to study the electrical activity of muscles. An MRI scan of the muscles may be advised. Sometimes, a skin or muscle biopsy may be needed.
Treatment
This condition cannot be cured; treatment is aimed at providing symptomatic relief. The commonly used medications include corticosteroids, antimalarial drugs and medications used for rheumatoid arthritis. Speech therapy and physical therapy are recommended.
Intravenous immunoglobulin therapy is one of the treatment options in which healthy antibodies from a pool of donors are infused into the patient’s bloodstream. Surgical intervention may be necessary to remove calcium deposits.