Causes and risk factors
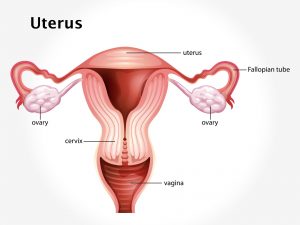
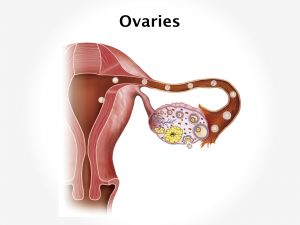
Endometrial hyperplasia is classified according to the pathology. Simple hyperplasia is abnormally thickened endometrium with presence of an increased ratio of glands to stroma; the glands are cystically dilated and somewhat irregular with some infolding and budding. Complex hyperplasia represents glandular crowding with even less intervening stroma and the glands show significant infolding and budding. Atypical hyperplasia refers to either simple or complex architectural patterns in which the cells lining the glands show loss of polarity, nuclear enlargement with increased nucleus-to-cytoplasm ratio and prominent nucleoli and irregularly condensed chromatin. Exact cause of endometrial hyperplasia is unknown. Hormonal changes in endometrial hyperplasia include increase in estrogen levels without progesterone resistance. Genetic mutation within cells in the endometrium can lead to the disease condition. Endometrial hyperplasia is associated with a history of unopposed estrogen exposure, either exogenous such as long term use of OC pills or endogenous. In premenopausal women it is associated with obesity and anovulation. Therefore, women with known polycystic ovary syndrome or known anovulation are at increased risk for developing this disease. Additional risk factors for developing this disease are nulliparous women, women having history of precocious puberty, delayed menopause, or those who have had radiation therapy to the pelvis, women with history of endometrial polyps, diabetes, and irregular periods.
Clinical presentation
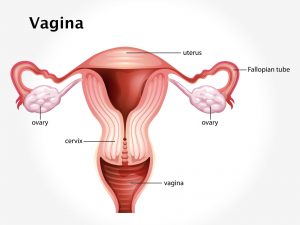
Endometrial hyperplasia is considered as precancerous condition. Irregular vaginal bleeding is the chief symptom of endometrial hyperplasia. Patient complains of bleeding between periods. There can be spotting after menopause. Prolonged, heavy, or frequent episodes of vaginal bleeding after age 40; thin, white, or clear vaginal discharge is experienced. Associated symptoms include lower abdominal pelvic pain, painful intercourse, and pain or difficulty when emptying the bladder.
Investigation
Medical history by the patient and clinical examination by the gynecologist helps in diagnosis. USG abdomen and pelvis is done. Atypical glandular cells of undetermined significance [AGUS] should be evaluated. Endometrial biopsy confirms the diagnosis.
Treatment
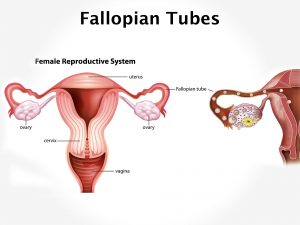
Treatment for endometrial hyperplasia depends upon histologic criteria, predisposing factors, patient age, and desire to maintain fertility. Treatment involves progestin therapy, oral contraceptives in women before menopause who do not desire to conceive. D&C should be performed to rule out malignancy. In those patients with persistent hyperplasia, definitive surgery should strongly be considered. Post-menopausal women will opt for a hysterectomy and bilateral salpingo-oophorectomy when there is risk of adenocarcinoma.
Other Modes of treatment
The other modes of treatment can also be effective in treating endometrial hyperplasia. Homoeopathy is a science which deals with individualization and considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly, the Ayurvedic system of medicine which uses herbal medicines and synthetic derivates is also found to be effective in treating endometrial hyperplasia.
Recent updates
An experimental approach for treating endometrial hyperplasia is going on with insertion of an intrauterine contraceptive progesterone system [ICPS], which releases continuous therapeutic doses of progesterone or levonorgestrel.
Facts and figures
The risk of development of cancer in patients with endometrial hyperplasia was 1% for patients with simple hyperplasia without atypia, 3% for those with complex hyperplasia without atypia, 8% for those with atypical simple hyperplasia, and 29% for patients with complex atypical adenomatous hyperplasia.


![Lobular Carcinoma In Situ [LCIS]](https://moho.loopshell.com/read/wp-content/uploads/2022/01/Lobular-Carcinoma-In-Situ-Lcis-300x300.png)