Causes and risk factors
Fungal infection spreads from other parts of body to joints. Hematogenous spread of infection occurs. Use of contaminated instruments during surgery can cause spread of fungal infection to joints. Common diseases that predispose to fungal arthritis are candidiasis, coccidiosis, blastomycosis, histoplasmosis, sporotrichosis, cryptococcosis, aspergillosis. Patients with diabetes, TB, alcoholism, and prolonged use of steroids are at high risk of developing the disease. People with weakened immune system are also susceptible.
Clinical presentation
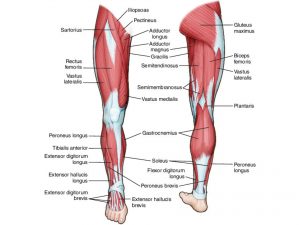
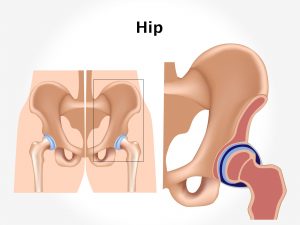
Symptoms of fungal arthritis include pain and inflammation of joints. Swelling of the ankles, feet, and legs occur. There is joint stiffness, joint swelling. Fever may be present. Underlying fungal infection is the characteristic of the disease.
Investigation
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Culture of joint fluid is required. X-ray of joint is advised. Serology test [positive for fungus] is recommended. Synovial biopsy is done.
Treatment
Treatment involves administration of antifungal drugs. Surgery may be required to remove the infected tissue. Symptomatic treatment such as analgesic, NSAIDs are given.
Other Modes of treatment
The other modes of treatment can also be effective in treating fungal arthritis.
Homoeopathy is a science which deals with individualization and considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly, the Ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating fungal arthritis.