Causative and risk factors
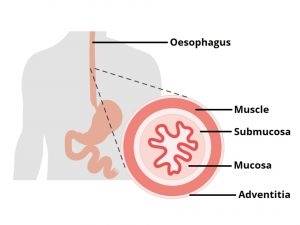
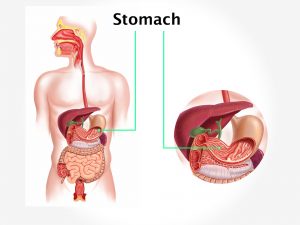
There is a valve located at the junction of the esophagus and the stomach that allows the esophageal contents to pass into the stomach but not vice-versa. Sometimes this valve starts functioning abnormally, thus allowing the stomach acids and contents to backwash into the esophagus.
Factors that make GERD worse include obesity, pregnancy, having large meals, fatty or spicy foods and lying down or bending over soon after a meal. Consuming alcohol, caffeine, carbonated beverages, fruit juice, chocolate or peppermint, certain medications, smoking or using tobacco products also worsens GERD.
Clinical presentation
The most common symptom of GERD is heartburn or a burning sensation in the chest region. The patients may have dysphagia (difficulty in swallowing) or odynophagia (pain with swallowing). There may be a sensation of a lump in the throat. Other symptoms include excessive secretion of saliva, nausea, hoarseness and a sore throat.
Investigation
The diagnosis of GERD is suspected on the basis of the patient’s symptoms alone. Certain tests may be carried out for confirmation. A barium swallow can demonstrate acid reflux. Endoscopy is carried out to look for any signs of damage in the lining of the esophagus or the stomach. Other tests include X-ray of your upper digestive system, ambulatory acid (pH) probe tests and esophageal motility testing
Treatment
Treatment includes lifestyle measures, medications and surgery if necessary. Lifestyle measures include losing excessive weight, avoiding spicy and citrus food, having small meals, drinking plenty of water and maintaining an adequate time gap between eating and lying down.
Medications include the use of antacids, H2 receptor blockers, proton pump inhibitors and prokinetic agents.
Surgical intervention is necessary in patients who are not relieved with lifestyle measures and medications.