Causes and risk factors
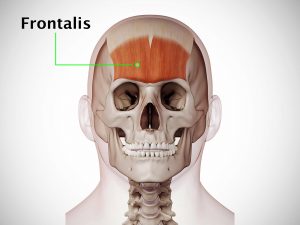
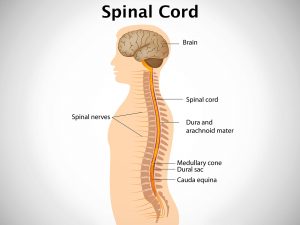
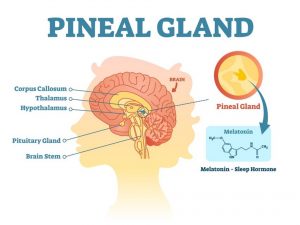
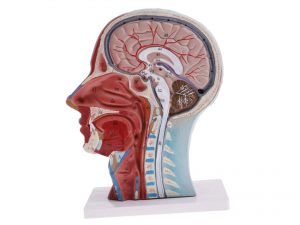
The causes of Horner’s syndrome include trauma to the base of skull, stroke, middle ear infection. Pancoast tumour, syringomyelia, cluster headache, spinal cord injury can lead to the disease. Disorders like goiter, thyroid carcinoma, multiple sclerosis, Klumpke paralysis, cavernous sinus thrombosis can cause Horner’s syndrome.
Clinical presentation
It is characterized by a triad of drooping upper eyelid [ptosis], pupil constriction [miosis] and absence of sweating on one side of the face [hemifacial anhidrosis]. Patient of Horner’s syndrome present with symptoms on only one side of the body. They include redness of conjunctiva, partial ptosis, decreased pupil size of the affected eye, enophthalmos [sinking of eyeball into the face]. There can be reduced sweating on the affected side of the face [anhidrosis].
Investigations
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Cocaine drop test is done where cocaine drops are instilled into the eyes. The pupils fail to react to the drops, i.e., no dilatation is seen. Diagnosis is presence of Horner’s syndrome. Other tests include blood and urine test. Chest x-ray is advised. Imaging studies such as MRI of head, neck, and chest may be useful for further evaluation.
Treatment
There is no specific treatment for Horner’s syndrome. It disappears on its own once the underlying cause is treated.
Complications
Horner’s syndrome itself does not cause any complication.
When to Contact a Doctor
One must consult a doctor if there is abnormality in sensory and motor functions of the eye and face.
Prevention
There is no sure way to prevent Horner’s syndrome.
Systems involved
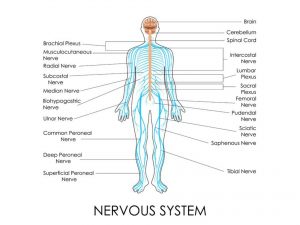
Central nervous system
Organs involved
Eye, face