Causative and risk factors
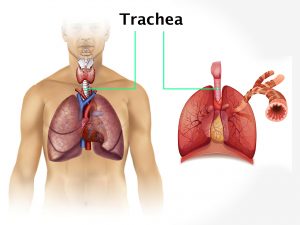
Hypercalcemia is mainly caused due to overactivity of parathyroid glands. Certain types of cancer, especially lung and breast cancer and also some cancers of blood increase the risk of hypercalcemia. Long period of immobilization are associated with a risk of developing hypercalcemia. Hyperthyroidism or excessive thyroid hormone intake are known risk factors. Other causes of hypercalcemia include inherited kidney or metabolic conditions, kidney failure and dehydration. Side-effects of certain medications and excessive vitamin D or calcium intake can also lead to hypercalcemia.
Clinical presentation
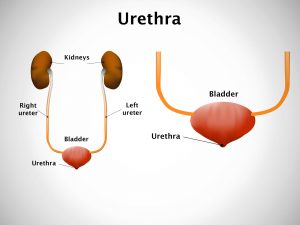
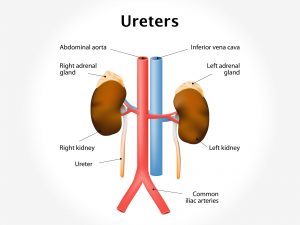
If you have mild hypercalcemia, then you may have few or no symptoms. Symptoms of severe form of hypercalcemia include excessive thirst, excessive urination, nausea, vomiting, decreased appetite, constipation, weakness, bone pains and abdominal pain. He/she may experience pain between your back and upper abdomen on one side. The patient may develop kidney stones, peptic ulcer disease, bowed shoulders, curvature of the spine and fractures.
Other symptoms include confusion, dementia and memory loss.
Investigations
Blood test is done to check the calcium and parathyroid hormone level in your blood.
Certain tests are ordered to determine other underlying causes of hypercalcemia. They include chest X-ray, CT or MRI scans and a mammogram.
Treatment
People with severe hypercalcemia, need to be hospitalized. The treatment is focused on getting the calcium levels to normal and preventing damage to bones and kidneys. Treatment may include intravenous fluids and medications. Calcitonin is given to slow down bone loss. Corticosteroids may be prescribed. Dialysis is recommended, if kidneys are damaged.
After bringing down the calcium levels to normal, treatment of hypercalcemia includes treating the cause.