Causes and risk factors
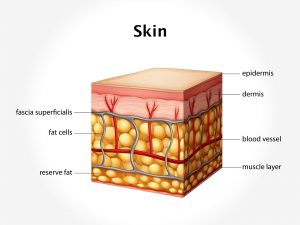
Hypopigmentation can be localized or generalized. It can be genetic or due to hormonal changes. Partial loss of melanocyte function occurs with loss of skin color. It is caused by an absence of melanocyte stimulating hormone [MSH]. It is seen in hypopituitarism. It is a localized hypopigmentation due to hormonal changes. Localized depigmentation is most commonly seen in vitiligo. Positive family history is often found in vitiligo. Trauma to the skin such as burns, skin infection, blisters, and scalds can also cause localized hypopigmentation.
Genetic causes include diseases like albinism. In albinism, an autosomal recessive condition, there is reduced or absence of production of melanin with loss of pigment from the skin, hair, and eyes. This is generalized hypopigmentation due to genetic causes. Other genetic conditions with loss of skin pigment include piebaldism, phenylketonuria, and tuberous sclerosis. Other causes of hypopigmented lesions include postinflammatory conditions after psoriasis, eczema, lichen planus, and lupus erythematosus; infections, for example, tinea versicolor and leprosy; chemicals, reactions to pigmented nevi, etc.
Clinical presentation
Hypopigmentation of vitiligo consists of sharply demarcated, symmetrical macular lesions. These are smooth, white patches on the skin. They gradually appear all over the body. In albinism there is complete loss of pigmentation in skin, hair, and eyes. Pityriasis alba lesions include several round or oval, scaly pink patches usually on the cheeks and arms. Pityriasis versicolor patches appear on the trunk, neck, and arms. Patches are coppery brown in color. Mild itching may be present. Lesions of lichen sclerosis occur as white, crinkled, thickened patches. It is common in perianal and genital areas. Leprosy patches are varied in presentation. As a general rule, they are asymmetrical lesions with loss of sensation.
Investigation
Medical history by the patient and clinical examination by the dermatologist helps in diagnosis. Skin biopsy may be done. Complete blood count is advised. Thyroid function tests to test thyroid levels is recommended. Tests to detect antinuclear antibodies to detect presence of any autoimmune disease is done.
Treatment
Treatment depends upon the underlying cause. No treatment is required for patients, with hypopigmentation developed as a result of burns or trauma. Hypopigmentation due to hormonal changes require hormone replacement therapy. In case of vitiligo, use of corticosteroid creams or ointments on the depigmented patches is effective, especially if treatment is begun in the initial stages. Topical ointments are effective for people with small areas of depigmentation, especially on the face and neck. Use of PUVA [topical psoralen plus ultraviolet A] therapy will also help in managing hypopigmentation of vitiligo. Excimer laser can be used to deliver UVB light to small areas of the skin. Narrowband ultraviolet B [UVB] therapy, depigmentation therapies are also useful. Surgery involves skin grafts which are used for small depigmented areas. Tattooing can be an option for people who want to cover up the affected parts of skin.
Other Modes of treatment
The other modes of treatment can also be effective in treating hypopigmentation. Homoeopathy is a science which deals with individualization and considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly, the Ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating hypopigmentation.