Causes and risk factors
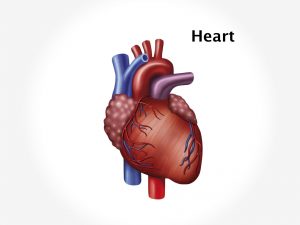
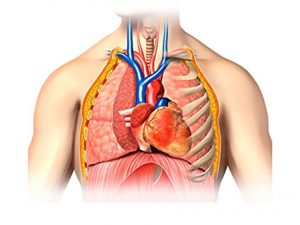
The exact cause of HLHS is not known. It is due to changes in genes or chromosomes. It occurs when heart is developing during foetal growth. The left side of heart which pumps blood to the entire body is not developed properly. This causes reduced blood supply to the body. The right side of heart maintains circulation in the body [pumping of blood to lungs as well as to the entire body] through two following conditions which are present normally at birth but disappear shortly after birth – ductus arteriosus and foramen ovale. Ductus arteriosus is a blood vessel that is present in all foetuses while in the womb that allows blood to bypass the pathway to the lungs; in HLHS, it allows blood to flow from the pulmonary artery to the aorta for some period till the ductus arteriosus is open. The blood returning to heart from lungs passes through the patent foramen ovale [a hole connecting the collecting chambers on the left and right sides of the heart] back to right side of heart. As the ductus arteriosus and foramen ovale starts closing it increases the load on right side of heart. The Risk factors responsible for development of the deformity are age of mother [above 40], maternal nutrition, alcoholism, gestational diabetes, viral disease during pregnancy like rubella, family history of CHD or Fallot’s tetralogy.
Clinical presentation
Many times patient is asymptomatic for few days after birth. Gradually the child shows symptoms like laboured feeding, the child tires easily, has shortness of breath, and has heavy or rapid breathing, has a poor appetite, and no weight gain. Symptoms of pulmonary hypertension such as cough, dyspnoea may be present. Additional signs such as Heart murmur, increased heart rate, prolonged crying, irritability, palpitations, central cyanosis [ blue discolouration of lips, tongue] help in suspecting a CHD.
Investigation
Medical history by the patient’s parents and Clinical examination of the child by the paediatrician helps in diagnosis. A cardiac murmur can be easily heard on a stethoscope on auscultation which will diagnose CHD. Pulse oximetry measures amount of oxygen% in the blood. A CBC, chest X ray, ECG is done. Echocardiography, cardiac catherization will confirm the diagnosis.
Treatment
Treatment Involves only surgical correction of the defective heart. Progressive hypoxemia and recurrent cyanotic spells indicate immediate surgery. Immediate hospitalisation of the patient in intensive care unit is necessary. Medicines such as prostaglandins are given to keep the ductus arteriosus open and keep blood circulation in the body. A ventilator may be required. Surgical Treatment i.e. stage I treatment involves a ‘Norwood operation’ which consists of reconstruction of aorta. Stage II treatment consists of ‘Glen shunt’ procedure which connects superior vena cava directly to pulmonary arteries. Stage III is the Fontan procedure which involves connecting inferior vana cava to the blood vessels of lungs. Post surgery, antibiotics to prevent any infections, avoidance of physical exertion in children, will also help in managing the patient.