Causes and risk factors
Lymphogranuloma venereum (LGV) is caused by bacteria Chlamydia trachomatis. The bacteria are transmitted by having unprotected sex (vaginal, anal, or oral) with the infected person. The bacteria can also gain entry into the body through break in the skin.
Clinical presentation
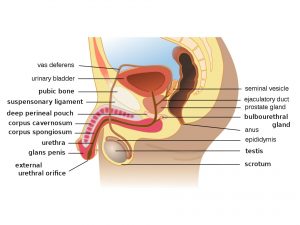
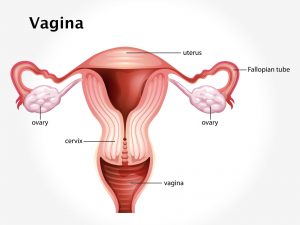
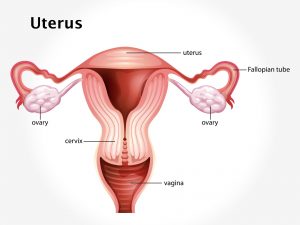
Symptoms of LGV occur in three stages: – Stage 1 – there occur painless papule or pustules. Common sites of infection for men include the prepuce, glans, and scrotum. Common sites of infection in women include the posterior vaginal wall, posterior cervix, fourchette, and vulva. The lesion ulcerates, heals, and disappears within a few days and may go unnoticed. Stage 2– More common in males than females. Swollen lymph nodes (lymphadenopathy) appear on both sides of groin about 1-2 weeks after stage 1. Enlarged lymph nodes are painful and tender. Associated symptoms include fever, chills, malaise, myalgia, and joint pain. Stage 3 – More common in females as compared to males. Symptoms are suggestive of proctocolitis. Symptoms include fever, pain on urinating and passing stool, bloody diarrhea, rectal pain, and tenesmus. In females, cervicitis, perimetritis, or salpingitis may occur, as well as there can be lymphangitis and lymphadenitis in deeper nodes. As disease progresses, buboes are formed. Chronic inflammation may lead to abscesses, fistulas, lymphatic obstruction, and rectal strictures. Chronic infection can cause scarring of the genitals.
Investigations
Medical history by the patient and clinical examination by the dermatologist helps in diagnosis. Recently, a fast real-time PCR (TaqMan analysis) has been developed to diagnose LGV. Lymph node biopsy is recommended.
Treatment
Treatment involves antibiotics for 3 weeks to fight the infection and prevent tissue damage. Drainage of the swollen buboes may be required to reduce discomfort. Surgical intervention such as repair of fistula, dilatation of the rectal stricture, and colostomy for rectal obstruction will contribute further to the treatment.
Complications
Complications such as genital elephantiasis, proctocolitis, arthritis, pneumonitis, hepatitis if there is systemic spread can occur.
When to Contact a Doctor
One must consult a doctor if he develops signs and symptoms similar to LGV such as papules, pustule on genitals, and has a history of unprotected sex.
Prevention
Safe sex practices such as protected intercourse, avoiding sex with high risk individuals prevents the disease.
Systems involved
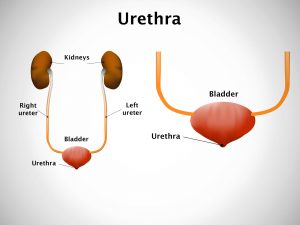
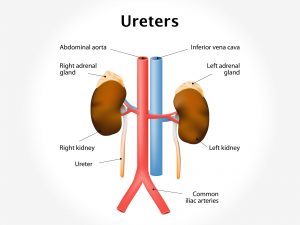
Genitourinary system, lymphatic system, integumentary system, GIT.
Organs involved
Genitals, lymph nodes, rectum, anal canal.