Causes and risk factors
The cells undergo an abnormal and uncontrolled proliferation. Eventually, these clusters of cells lead to formation of a tumor or mass. What causes this abnormal growth is still a mystery. However, tedious research and study of various cases have laid down certain risk factors which can predispose a person to cancer. Genetic factors head the list. Many cancers are caused due to certain abnormality or mutation in the genes which stimulate the cells to undergo an abnormal proliferation. Certain infections can predispose one to vulvar cancers – human papilloma virus is the most common among it. Among those, infection due to HPV strain 16 and 18 are more commonly seen. This viral infection spreads during sexual intercourse. Immuncompromised females along with women who smoke are also at high risk of developing cancers. Vulval lichen planus, Paget’s disease of the vulva, and lichen sclerosis increase the risk. Vulval intraepithelial neoplasia is said to be precursor for cancer of vulva. Vulvar cancers can be due to metastasis of a malignant condition present elsewhere in the body.
Clinical presentation
There are different types of vulval cancers – squamous cell carcinoma, adenocarcinoma, verrucous carcinoma, sarcoma, basal cell carcinoma and vulval melanoma/carcinoma.
Indolent growth of abnormal cells in its initial stage does not pose any noticeable signs and symptoms in the body, hence the patient remains asymptomatic, and most of the times the tumor is accidentally detected while conducting other procedures or surgeries. Some people over a period of time can come up with other health issues. On most of the occasions, the patient usually comes up with vague symptoms like bodyache, fatigue, and tenderness all over the body. A noticeable change in weight is complained by the patient or is brought into notice by the loved ones. Some people can come up with complaints of pain during sexual intercourse or pain while passing urine along with burning, itching, and soreness. Bleeding or abnormal discharges from the vagina other than the menses can occur. Changes in color of the vulva along with ulceration or a lump like growth and swelling can be seen.
Investigations
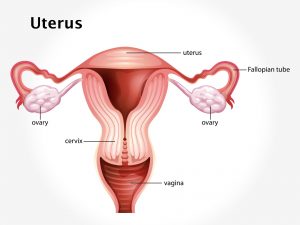
Diagnosis is done on the basis of the symptoms narrated by the patient and the rectovaginal examination carried out by the gynecologist. Endoscopy (hysteroscopy) for internal visualization of the uterus and Pap smear are done. Biopsy is the diagnostic investigation. Transvaginal or abdominal sonography, MRI, and CT scan can be done. In addition to these, routine blood, CA-125 blood test, and PET scan for metastasis are advised.
Treatment
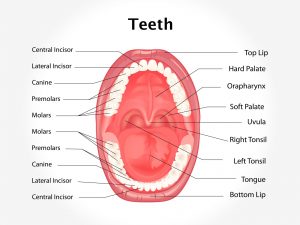
Depending upon the extent and stages of cancer, the treatment is planned. Various surgical approaches can be adopted. Excision of the tumor or vulvectomy is done. Hysterectomy is found to be effective in cases where metastasis has occurred. Radiation therapy is used. Targeted chemotherapy and immunotherapy agents are administered. Along with the above-mentioned treatment, certain preventive measures need to be implemented. All sexually active women should get vaccinated against human papilloma virus and use barrier contraceptive devices during sexual intercourse, e.g., condoms and use barriers for oral sex, e.g., dental dams. Regular Pap smears should be done. In women between the ages of 21-29, it should be done after every 2 years and in women after the age of 30, it should be done after every 3 years.