Causes and risk factors
In most cases of mitral valve prolapse the cause is unknown. But in some cases it may be a genetically determined collagen tissue disorder associated with rheumatic heart disease, ischemic heart disease, atrial septal defect or hypertrophied cardiomyopathy. Mitral valve prolapsed can also occur in association with Marfan’s syndrome, Ehlers Danlos syndrome, thyrotoxicosis, lupus or Ebstein’s anomaly.
Clinical presentation
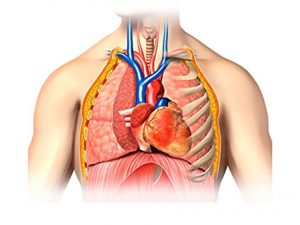
In mitral valve prolapsed, there is leakage of blood back into the left atrium when the heart contracts. This leakage of blood is called as mitral regurgitation. When the amount is small it is harmless and most people are not aware about it. However some people may experience symptoms like chest pain and palpitations. The patient may be dizzy, tired and experience shortness of breath worse lying down (orthopnea) and on exertion.
Complications of MVP include regurgitation, endocarditis, arrhythmias and transient ischemic attack.
Investigations
Based upon your symptoms your doctor will perform physical examination and order investigations to confirm the diagnosis of mitral valve prolapse.
During physical examination, your doctor will auscultate your chest area using stethoscope. He/she may hear a clicking sound as well as heart murmur if you have MVP.
Investigations include chest X-ray, ECG, echocardiogram and Color Doppler studies.
Treatment
Asymptomatic patients do not require any treatment except for reassurance. Patients who have symptoms will require the use of aspirin, beta blockers and other medications. Antibiotics are given to prevent endocarditis before any dental procedure.
In severe cases surgery to repair or replace the valve is performed.