Causative & risk factors
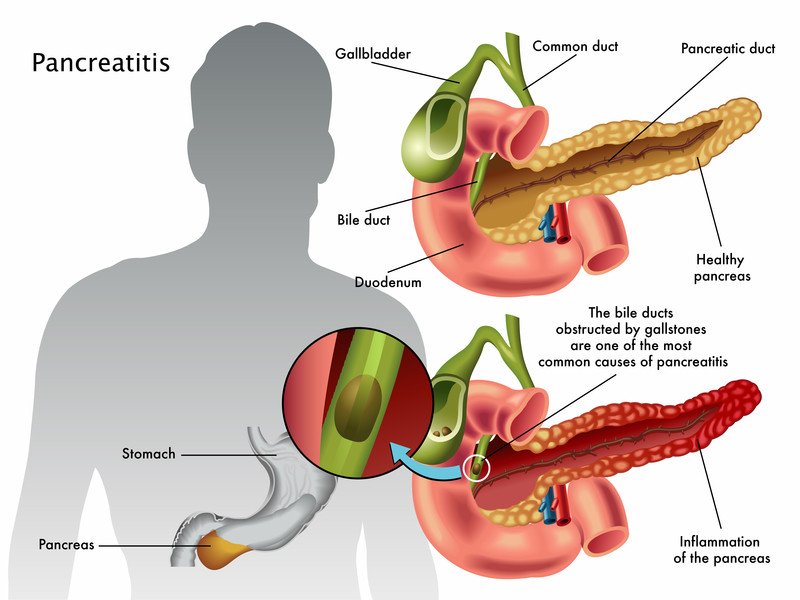
Abuse of alcohol has been identified as a major cause of pancreatitis. Other risk factors include smoking, a family history of pancreatic disease, history of injury or surgery on the abdomen and having high triglyceride levels in the blood. Certain underlying diseases such as cystic fibrosis, gallstones, obstruction of the bile ducts or pancreatic cancer predispose to pancreatitis.
Clinical presentation
Acute pancreatitis presents with sudden, severe pain (sharp/stabbing in character) in the upper abdomen which worsens after eating. This pain may also radiate to the back. The patient also experiences nausea and vomiting and his abdomen will be tender to touch.
Chronic pancreatitis also presents with upper abdominal pain. The patient loses weight and passes fatty stool (steatorrhea).
Untreated pancreatitis can cause several complications such as infection of the pancreas, formation of a pseudocyst or pancreatic cancer. It can also affect other body systems giving rise to kidney failure, malnutrition, breathing problems and diabetes.
Investigations
After an initial assessment of the patient, the levels of pancreatic enzymes (serum amylase, serum lipase) in the blood are tested. An ultrasound, CT scan or MRI scan is suggested which will reveal abnormalities of the pancreas and surrounding structures. The patient’s stool is tested to detect the presence of fats.
Other general blood tests are recommended such as fasting blood sugar, liver function tests, kidney function tests etc. to detect any other co-existing abnormality. The serum electrolyte levels of the patient must be monitored, especially in cases of acute pancreatitis.
Treatment
Any patient with suspected pancreatitis must be admitted in a hospital. Oral feeds are stopped immediately and the patient is given nutrition intravenously for a few days. Painkillers are prescribed to relieve the pain. Once the cause of pancreatitis is confirmed, specific treatment for the cause begins. This may include any of the following:
Cholecystectomy – removal of the gallbladder
ERCP (endoscopic retrograde cholangiopancreatography) – to visualize and remove bile duct obstruction
Surgery to remove part of the pancreatic tissue
In the long term, certain measures are advised to the patient especially those who suffer from chronic pancreatitis. Alcohol must be completely restricted. One can opt for professional de-addiction programs. The dietary fat content must be kept low while maintaining an otherwise nutritious diet. Pancreatic enzyme supplements are prescribed in the form of tablets.
Recent updates
Recent studies have suggested that histamine drugs may be used in the treatment of pancreatitis.