Causative & risk factors
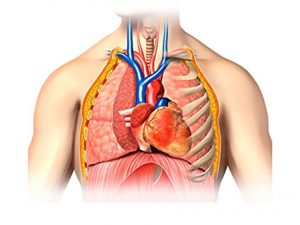
The cause of pericarditis is not clear in most cases. A viral infection is one of the suspected causes. Pericarditis can occur as a sequel to a heart attack. It can also result from rheumatic diseases (SLE, RA), cancers, AIDS, renal failure of and intake of certain medications. Trauma to the chest can also cause pericarditis.
Clinical presentation
A sharp, stabbing pain is felt on the left side of the chest which may radiate to the shoulder or neck. The patient may experience palpitations, breathlessness, fatigue, fever and cough. Patients with chronic constrictive pericarditis usually develop pedal edema (swelling in the legs).
Dressler’s syndrome is a specific type of pericarditis that occurs several weeks after a heart attack or heart surgery.
Accumulation of excessive pericardial fluid can lead to the development of cardiac tamponade, a medical emergency.
Investigations
After a symptomatic assessment, the doctor will auscultate your chest to hear the typical ‘pericardial rub’ which is a sound produced by the friction of pericardial membranes.
Blood tests are carried out to detect evidence of infections. Imaging tests such as Chest X ray, ultrasound, CT or MRI scan are carried out to visualize the heart clearly. ECG (electrocardiogram) and 2D echocardiogram/Color Doppler are also carried out.
Treatment
Most cases of pericarditis are mild and self-limiting. Painkillers, colchicine and corticosteroid drugs are prescribed for relief.
In cases with cardiac tamponade, a procedure known as pericardiocentesis is carried out to extract and analyze the pleural fluid.
Pericardiectomy – a procedure to surgically excise the entire pericardium may be necessary in cases of constrictive pericarditis.
Recent updates
Idiopathic recurrent acute pericarditis (IRAP) is a rare disease which is diagnosed in lonf-standing cases of pericarditis where other infectious and noninfectious causes of pericardial inflammation have been ruled out.