Causative & risk factors
Psoriasis is an autoimmune disease; the exact cause remains unclear. The skin cells grow rapidly and pile up forming thick silvery scales and itchy, dry, red patches.This condition tends to run in families.
Although psoriasis can begin in any age group, adolescents and young adults are more commonly affected.
Psoriasis can be triggered by trauma, cold weather and certain types of medications. People with psoriasis are generally better during summer and worse in winter.
Clinical presentation
Psoriasis begins with the development of reddish, slightly raised eruptions which are topped with whitish scales. These eruptions eventually join together to form well-defined, raised plaques covered with thick silvery scales.
Prolonged remission periods are common in psoriasis.
Psoriatic patches can appear anywhere on the skin. However, the usual sites of affection are the scalp, knees, elbows, extensors of extremities and the sacrum in a symmetrical pattern. Palms and soles may also be involved. Apart from this classical presentation, psoriasis can sometimes affect certain specific body parts such as:
- Palmoplantar psoriasis – Palms and soles are involved
- Scalp psoriasis – Involving the scalp and extending beyond the scalp margins
- Inverse psoriasis – Involving the axillae and groin area
- Nail psoriasis – Involving the nails
- Guttate psoriasis – Involving the trunk, arms and legs. This form of psoriasis usually disappears within a few months.
- Pustular psoriasis – Crops of pustules are present on the affected locations
About 1 in 7 patients of psoriasis develop psoriatic arthritis. Psoriatic arthritis classically affects the finger joints, though sometimes other joints may also be affected.
Investigations
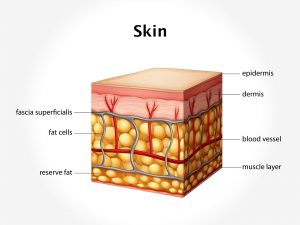
Physical examination of the skin is adequate to diagnose psoriasis. The physician usually performs the “Auspitz sign” to confirm psoriasis; in which removal of a scale leads to pinpoint bleeding in the underlying skin.
Skin biopsy may be carried out when the diagnosis is unclear.
Treatment
Psoriasis cannot be cured, but can only be managed.
Lifestyle changes – Steps must be taken to lose excess weight and avoid any kind of trauma to the skin. Any kind of strong soaps or perfumes must not be applied on the affected skin.
External applications containing emollients, urea, salicyclic acid, coal tar or steroids are advised.
Oral medications involve the use of retinoids, steroids, methotrexate etc.
Therapies for psoriasis are PUVA therapy and UV-B Phototherapy. PUVA therapy consists of oral intake of the drug psoralen, followed by exposure to UVA radiation. UV-B Phototherapy consists of exposure to UVB light, with no need of any oral medication.
Aternative treatment with homoeopathy is seen to have a very good scope in treating psoriasis.
Recent updates
Biologic agents are being explored as a treatment option for psoriasis. These agents work by blocking part of the immune system.