Causative and risk factors
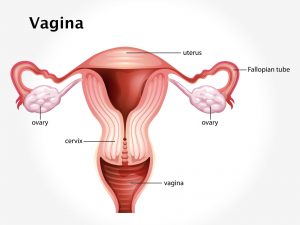
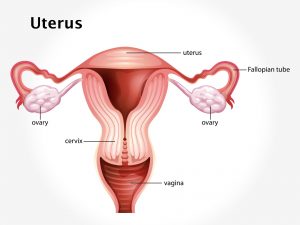
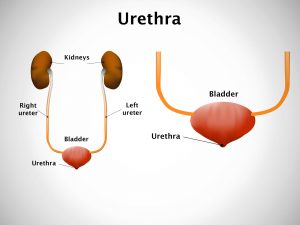
Q fever is caused by infection with the bacterium Coxiella burnetii. Infection is transferred to humans by inhaling aerosols from contaminated animal waste or contaminated soil. Contact with infected animals’ semen, vaginal mucus, feces, milk, and urine can cause Q fever. Ingestion of milk of infected species can transmit the infection. Infection can occur even with a single bacterium.
Clinical presentation
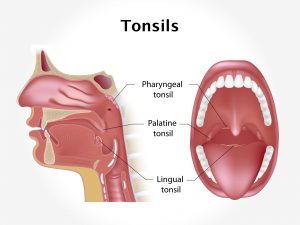
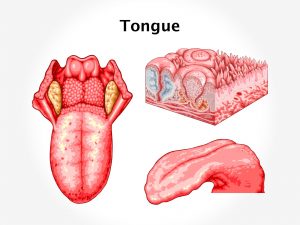
Symptoms develop 9-40 days after the infection. The patient may have a high fever, with or without chills, lasting for 7-14 days. Other symptoms include severe headache, profuse perspiration, malaise, myalgia, joint pains, chest pain and a dry cough. The patient loses his appetite and may complain of nausea, vomiting, diarrhea and pain in the abdominal.
Chronic Q fever can be seen in less than 5% patients. Immune-compromised people, pregnant women and people with heart valve disease are at higher risk.
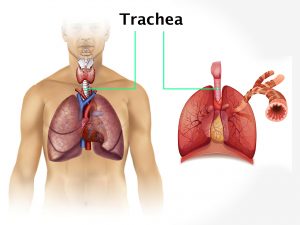
Q fever can give rise to complications like pneumonia, myocarditis, granulomatous hepatitis, thrombocytopenia, chronic fatigue syndrome and acute respiratory distress syndrome. There is an increased risk for pre-term delivery or miscarriage in pregnant women.
Investigations
Diagnosis is mainly based upon the symptoms given by the patient. Certain basic tests such as complete blood count, liver function tests etc. are performed. To confirm the diagnosis, PCR testing, indirect immunofluorescence assay and IgG-IgM antibody testing is done.
Treatment
Q fever is treated with antibiotics. In acute case treatment duration is 2-3 weeks. In chronic cases, long-term treatment is necessary. The outcome depends upon how quickly diagnosis is made and treatment is started. Q fever responds well to antibiotic treatment. Untreated endocarditis leads to fatal outcome.
In order to prevent Q fever, people in high risk occupations can opt for Q fever vaccine.