Causes and risk factors
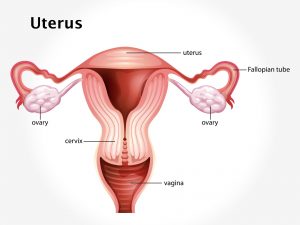
The small intestine and colon are susceptible to the acute effects of radiation. This is due to the rapid renewal rate of their epithelia. Radiation inhibits epithelial cell renewal in the exposed intestine. In the small intestine and colon this results in mucosal atrophy with decreased villus and crypt height in the small intestine and decreased crypt height in the colon and the rectum. In addition to this, mucosal inflammation occurs in the mucosa of both organs that lie in the field of radiation. Radiation enteritis is of 2 types – Acute radiation enteritis in which symptoms begin when radiation therapy is first given and up to 8 weeks after the therapy. Chronic radiation enteritis where symptoms begin several months to years after the radiation therapy.
Clinical presentation
Malabsorption is the main feature of radiation enteritis. The damaged segment of the small intestine is functionally impaired; however, there is less clinically evident malabsorption as there is sufficient unexposed small intestine to compensate and the mucosal lesion heals rapidly once radiation exposure stops. Diarrhea and hematochezia are common features of colitis and proctitis due to radiation therapy. Additional symptoms include nausea, vomiting, loss of appetite, cramping abdominal pain, frequent desire to have bowel movements, discharge of mucous from the rectum, rectal pain, and bleeding from rectum. Symptoms subside in 2-3 weeks after the radiation therapy is over. These symptoms also remit, in most cases, after radiation therapy has been completed. Symptoms of chronic radiation enteritis are wave-like abdominal pain, unintentional weight loss, bloody diarrhea, frequent desire to have bowel movements, bowel obstruction, and rectal bleeding. The delayed effect of radiation therapy to the intestine can cause serious debilitating disease.
Investigation
Medical history by the patient and clinical examination by the doctor helps in diagnosis. Complete blood count is done. Imaging studies such as endoscopy, colonoscopy, and capsule endoscopy may be useful for further evaluation.
Treatment
Treatment involves adequate hydration; medications such as anti-diarrheal, anti-emetics, and anti-spasmodics. Dietary modification involves – low-fiber diet. Foods to avoid are milk and milk products, whole wheat bread, fatty and greasy foods, nuts and seeds, raw vegetables, popcorn, highly seasoned foods and herbs, coffee and chocolate, alcohol and tobacco products. Foods to include in regular diet are – well cooked, broiled or roasted fish and chicken, bananas, apple and grape juices, eggs, white bread and toast, potatoes – baked, boiled or mashed, macaroni, mildly cooked vegetables, mild processed cheese, butter milk, and yoghurt. Surgical intervention involves intestinal bypass surgery in case where there is severe damage to the intestine.
Other Modes of treatment
The other modes of treatment can also be effective in treating radiation enteritis. Homoeopathy is a science which deals with individualization and considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly, the Ayurvedic system of medicine which uses herbal medicines and synthetic derivates is also found to be effective in treating radiation enteritis.