Causes and risk factors
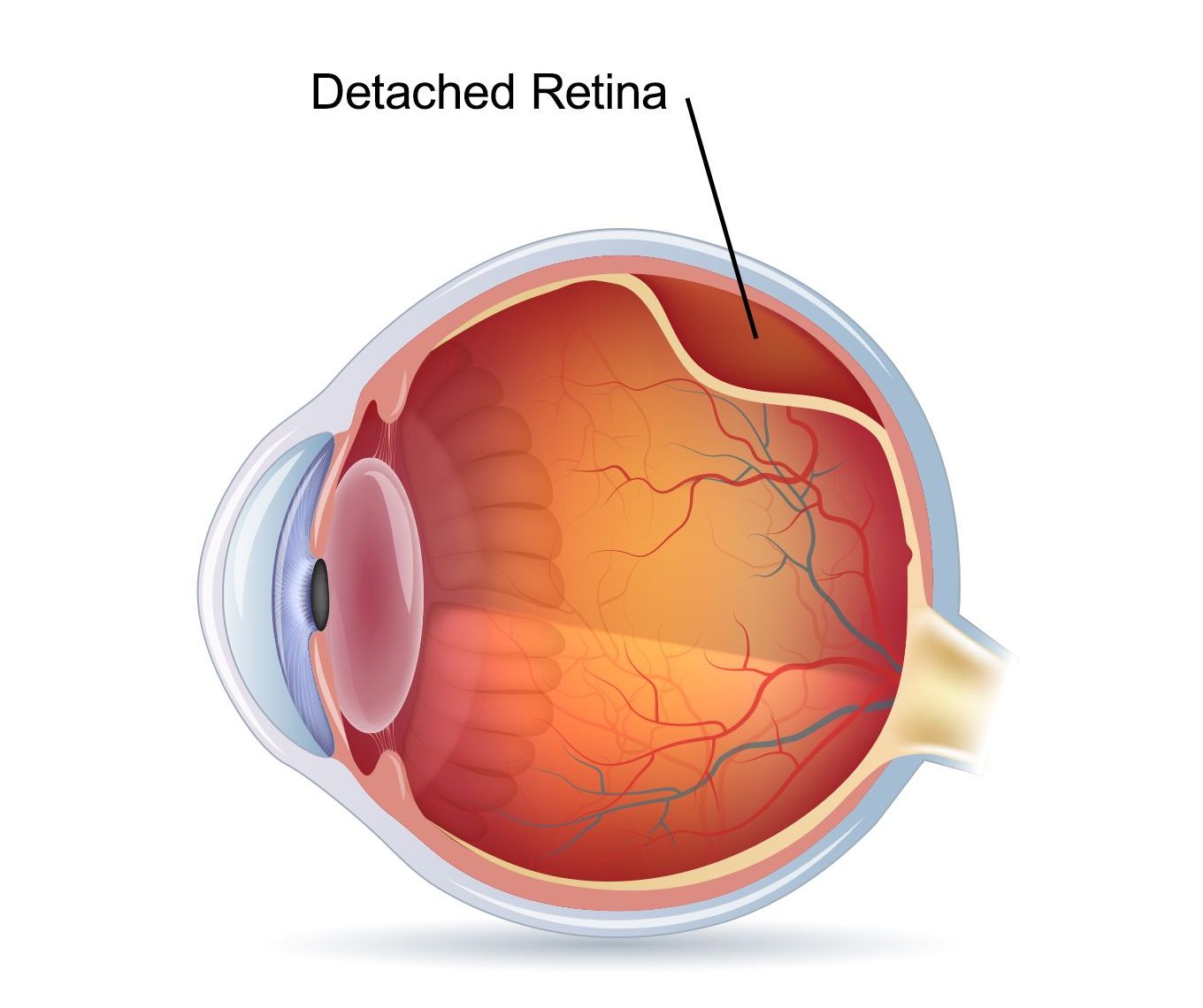
Retinal detachment can arise as a result of several eye conditions including severe myopia, eye injury, cataract surgery, uveitis, diabetic retinopathy, shrinkage of the vitreous, and retinoblastoma.
Clinical presentation
A patient with retinal detachment suddenly starts seeing floaters and flashes of lights in affected eye. There is a decrease in peripheral vision which progresses slowly to central vision. He may experience a sensation of curtain or shadow over field of vision. Straight lines now start appearing curved. Untreated cases can progress to blindness.
Diagnosis & Investigations
Based upon your symptoms, your doctor will examine your eyes to diagnose retinal detachment. The eye is examined using ophthalmoscope.
Retinal detachment must be differentiated from other eye conditions such as retinal artery occlusion, retinal vein occlusion, posterior uveitis and vitreous hemorrhage.
Treatment
Surgery is required to treat retinal detachment. Following are the options:
- Laser therapy
- Freezing therapy: if there is a tear in the retina and is diagnosed early.
- Pneumatic retinopexy: a small gas bubble is placed against the tear which puts pressure over the tear and closes it.
- Scleral buckle: a silicone band is sewed around the white of eye over the affected area
- Vitrectomy: in cases of large tear, the vitreous is removed and replaced with the saline solution
The outcome of retinal detachment depends upon the severity of the condition. It may take months after the treatment for vision to improve. In some cases the lost vision cannot be recovered even after the treatment.