Causative & risk factors
Shigella infection spreads from person to person through the faeco-oral route. Contaminated food or water are the common sources of infection.
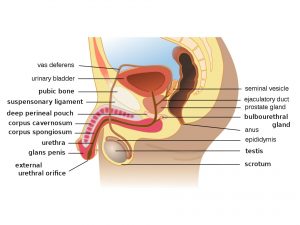
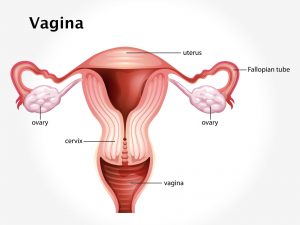
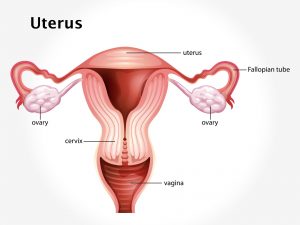
Sometimes shigellosis can occur due to person-to-person contact where fecal matter is involved. A parent getting infected by changing the diapers of an infected infant is a common example. Having unprotected anal intercourse with an infected person can also transmit the infection.
Clinical presentation
Some patients with shigellosis remain asymptomatic, whereas most will develop gastro-intestinal symptoms. Most patients will develop diarrhea, fever and cramping abdominal pain. The diarrhea is usually blood-stained. There may be discharge of pus or mucus in the stool.
Most patients with shigellosis usually recover entirely within a week. Some patients however may develop post-infectious arthritis. Other complications of shigellosis include dehydration, seizures, hemolytic-uremic syndrome, prolapse of rectum and toxic megacolon.
Some patients may never actually develop the symptoms of shigella infection, but only act as ‘carriers’. These carriers can go on transmitting the disease to others.
Investigations
A stool examination is done to identify the Shigella bacteria. Stool culture test may be advised to determine which antibiotic will work best for the patient. A complete blood count may be done.
Treatment
Antibiotics form the mainstay of treatment for shigellosis. Intravenous fluids and electrolytes are given to prevent dehydration.
They can sometimes be avoided if the symptoms are very mild and the patient is otherwise healthy.
Prevention is possible by:
- Frequent washing of hands.
- Hygienic handling of food during production, storage, cooking and eating.