Causes and risk factors
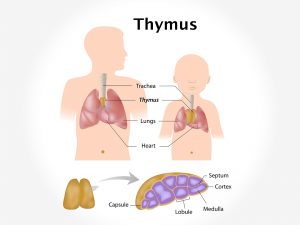
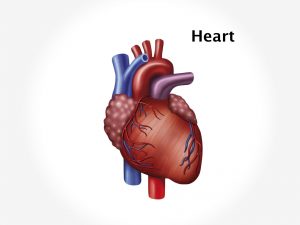
Heart rate is controlled by electrical signals passing across the heart tissues. Heart is made up of primarily muscle tissue. A network of nerve fibres regulates contraction and relaxation of heart muscles to obtain wave like pumping action of heart. Electrical signals are generated by SA node placed in the right atrium of heart. Autonomic nervous system controls the rate of signals sent by SA node. Electric signals follow the following pathway in the heart – SA node, Atrioventricular node, bundle of HIS, right and left bundle branch, purkinje fibres. AV node conducts impulses from atria to ventricles. In sick sinus syndrome, the heart doesn’t beat regularly causing rapid heartbeat [tachycardia], slow heart beat [bradycardia] or irregular heart beat. The diseases causing SSS include scarring of the heart tissue, history of previous heart surgery, and certain medications. People above 70 years of age, thyroid disease, history of previous MI, heart surgery, sleep apnoea, hyperkalemia are at risk of developing SSS.
Clinical presentation
SSS can present as sinoarterial block, sinus arrest or tachycardia bradycardia syndrome. In sinuarterial block electrical signals move too slowly causing bradycardia. In sinus arrest, activity of sinus node stops or is paused. In tachycardia bradycardia syndrome there is alternate fast and slow heart rate with a pause in between [asystole]. Signs and symptoms include dizziness, palpitations. Patient experiences light-headedness, anxiety, tiring during exercise, fatigue. Arrhythmia and tachycardia or bradycardias are the main alarming signs of the disease. Tachycardia arises in the upper chamber of heart. It involves atrial fibrillation, atrial flutter, and atrial tachycardia. Patient complains of chest pain, tightness of chest, shortness of breath. Disturbed sleep. Confusion may be accompanied symptoms.
Investigation
Medical history by the patient and Clinical examination by the doctor helps in diagnosis. it is diagnosed only during episodes of arrhythmia. Blood tests for potassium levels and thyroid hormones is recommended. An ECG is advised. Holter monitoring can be done [24 hours monitoring of electrical activity of heart]. Imaging studies such as chest X ray may be useful. Electrophysiological testing may be useful in the diagnosis of the condition.
Treatment
No treatment is required for asymptomatic patients. Regularising heart beat by methods such as vagal manoeuvre [putting ice pack on face, bearing down as if defecating or coughing] is required. Medications like anti arrhythmic drugs may be required to correct increased heart rate. When above treatment is not helpful, cardioversion is applied i.e. electric current is administered in the heart which restores normal heart rhythm. Surgical treatment to prevent tachycardia involves catheter ablation, pacemaker, implantable cardioverter defibrillator, open heart surgery.