Causes and risk factors
Sickle cell anemia is a hereditary disease caused by a genetic mutation. It is transmitted in an autosomal-recessive pattern which means that both parents must carry the defective gene in order for the offspring to develop sickle cell disease.
If only 1 parent carries the defective gene, the child becomes a carrier but does not develop the disease. However, he can pass on the defective gene to his offspring.
Clinical presentation
Sickle cell anemia gives rise to symptoms of anemia such as fatigue, breathlessness etc.
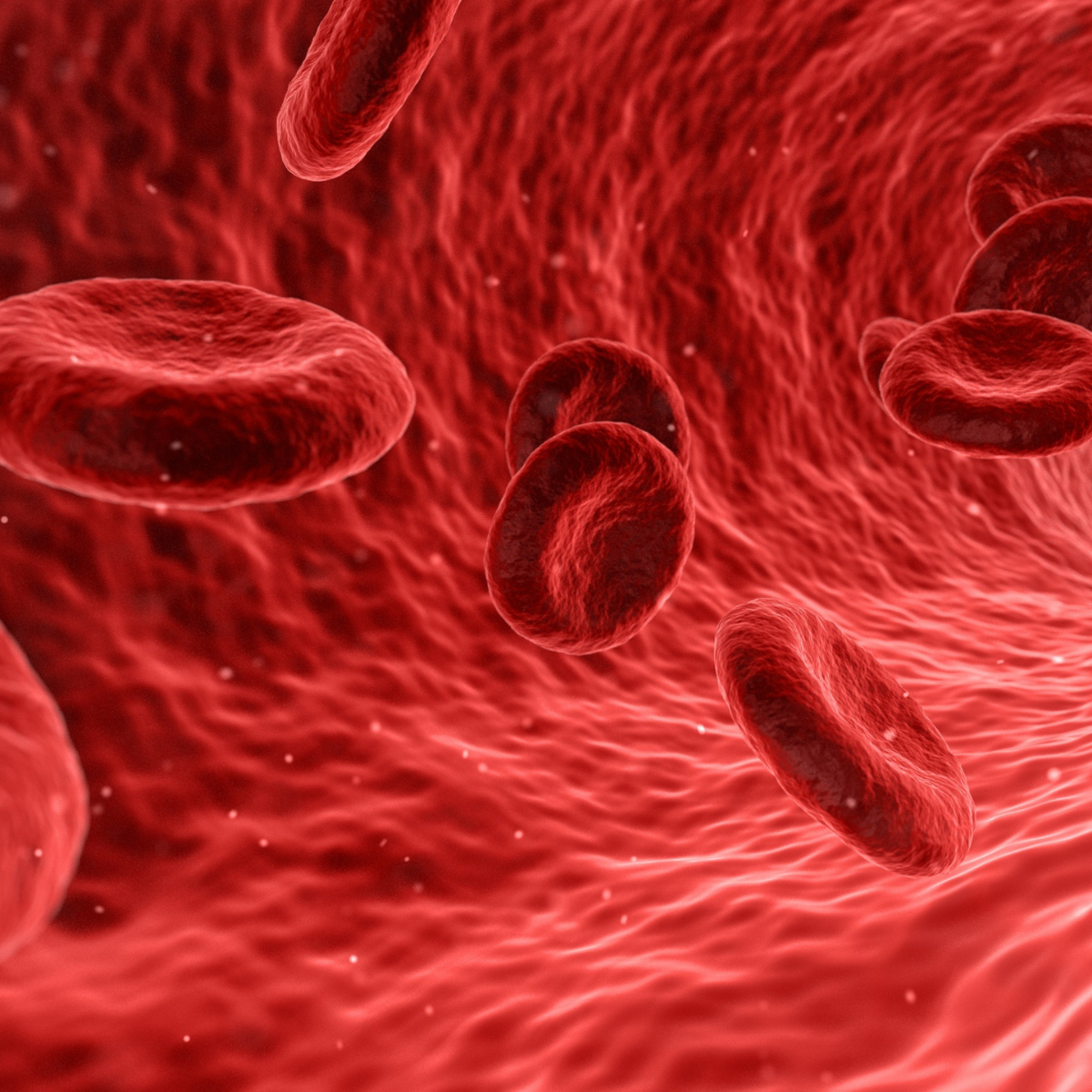
Sickle cell crisis: Sickle cells sometimes cause blockages in the blood vessels leading to organs or bones causing severe pain in the affected areas. Such episodes of pain are referred to as ‘sickle cell crises’. A person may have multiple such episodes every year.
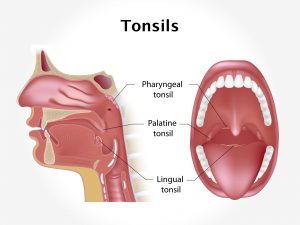
Sickle cells often cause damage to the spleen while passing through. Spleen being an important organ in maintaining immunity; a damaged spleen can lead to reduced immunity thereby causing frequent infections.
Dactylitis i.e. swelling of the hands and feet may be seen in infants. There may be ulcers on the lower limbs and visual defects due to blood vessel blockages.
Sickle cell anemia can give rise to complications such as frequent infections, stroke, visual defects, pulmonary hypertension, ulcers and organ damage.
Investigations
Sickle cell anemia must be differentiated from other causes of anemia such as iron deficiency, B12 deficiency or mal-absorption syndromes.
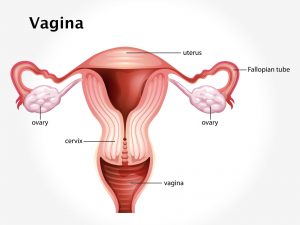
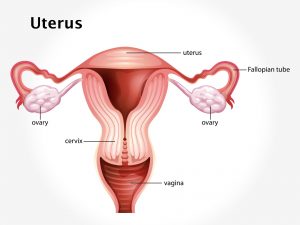
Sickle cell anemia can be confirmed by carrying out red blood cell count which will usually be low. A peripheral blood smear examination reveals a large number of sickle shaped cells. If sickle cell anemia is suspected in an unborn child, the amniotic fluid of the mother’s womb can be tested to look for the sickle cell gene.
Treatment
There is no cure for sickle cell anemia. The treatment revolves around managing symptoms and preventing complications. Over the counter painkillers are generally used during acute episodes of pain. Antibiotics are usually prescribed on a long term basis in order to prevent infections.
Hydroxyurea – This drug is usually given on long term basis to patients with sickle cell anemia. It helps to bring down episodes of sickle cell crisis.
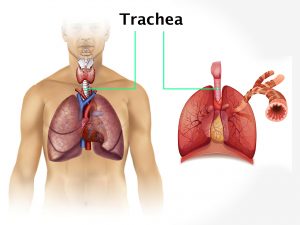
Blood transfusions are given as and when necessary. Oxygen therapy may be given, where oxygen is administered through a breathing mask.
Bone marrow transplant – Bone marrow from a matched healthy donor is transplanted to patients with severe sickle cell anemia. However, this can also cause several complications.
The life expectancy of people with sickle cell anemia is generally reduced. Some may die during infancy itself. Others may eventually succumb to complications involving their lungs, heart or other vital organs. With regular treatment, the life expectancy can be enhanced.
Those with a known family history of sickle cell disease must make sure that their spouse is free of sickle cell trait, before planning to conceive. Genetic counseling is helpful for this purpose.