Causative & risk factors
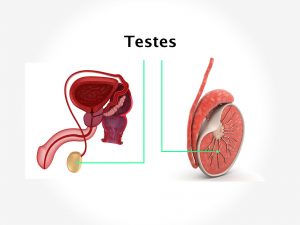
The exact cause of testicular cancer is not known but several risk factors have been identified. White men have a much higher risk of developing testicular cancer, so do men with a family history of this disease. History of undescended testicles is also associated with a higher risk of developing testicular cancer. This condition is also more common in men who are infertile and those who smoke.
Clinical presentation
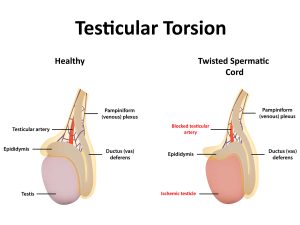
The commonest presentation of cancer in the testes is presence of a painless lump. Occasionally a sense of heaviness or a dull ache may be felt. Testicular cancer can produce a hydrocele.
Testicular cancer is staged as follows:
Stage 1 – the cancer is within the testicles
Stage 2 – the cancer has spread into the regional lymph nodes
Stage 3 – the cancer has spread into the lymph nodes at distant sites such as the chest
Stage 4 – the cancer has metastasized to other organs
Investigations
If your doctor suspects testicular cancer on the basis of physical examination, several tests will be carried out to confirm its presence.
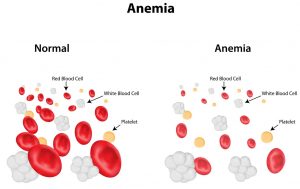
Blood samples are taken to test for markers of testicular cancer, which include Alpha feta protein (AFP), human chorionic gonadotrophin (HCG) and lactate dehydrogenate (LDH).
An ultrasound scan of the scrotum will be performed. Sometimes a CT or MRI scan may be needed. Testicular biopsy is a confirmatory test to detect testicular cancer.
Treatment
Compared to other forms of cancer, testicular cancer has a very good prognosis. Orchidectomy i.e. surgery to remove 1 or both the testicles is the treatment of choice. The regional lymph nodes may or may not be removed depending upon the spread of cancer. Surgery is followed by radiation therapy, chemotherapy or both.
Recent updates
Recent research has found several genetic variations that are present in men with testicular cancer. These will help identify men who are at a high risk of developing cancer of the testes. Role of stem cell transplant is also being studies for men suffering from testicular cancer.