Causative & risk factors
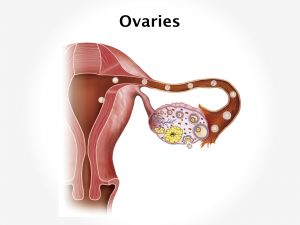
Any condition that causes weakening or loosening of the pelvic tissues and ligaments can cause prolapse of the uterus. These include obesity, advancing age, history of multiple vaginal deliveries or a major surgery in the pelvic region.
Conditions which lead to increased pressure in the abdomen such as chronic cough, constipation, pelvic tumors etc can also lead to uterine prolapse.
Clinical presentation
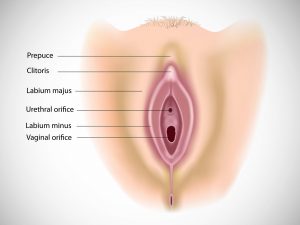
The patient will experience a sense of heaviness in the vaginal region and lower abdomen. She may feel a dragging down sensation in the pelvis. She starts experiencing sudden urges to urinate and may also suffer from urinary incontinence and frequent bladder infections. The uterus and cervix may bulge into the vaginal opening and intercourse may become difficult. Low backache is usually present. Discharge (sometimes bloody) from the vagina may be occasionally present.
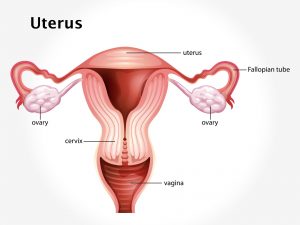
Uterine prolapse will be classified into various degrees such as:
- First degree: Only the cervix drops into the vagina.
- Second degree: The cervix sags to the level just inside the opening of the vagina.
- Third degree: The cervix is prolapsed outside the vagina.
- Fourth degree: The entire uterus is outside the vagina (procidentia).
Investigations
Diagnosis can be made on the basis of patient history and a pelvic examination.
Treatment
Lifestyle modification like weight loss, avoiding heavy weight lifting will help. Kegel’s exercises will help to tone up pelvic muscles. Use of pessaries is recommended. A pessary is a device inserted into the vagina to stabilize the uterus and cervix. Estrogen replacement therapy may be considered.
Surgery may be carried out to put the uterus back into its original position; although this is not recommended in women who plan to have children in the future. Hysterectomy (removal of the uterus) may be recommended to some women.


![Lobular Carcinoma In Situ [LCIS]](https://moho.loopshell.com/read/wp-content/uploads/2022/01/Lobular-Carcinoma-In-Situ-Lcis-300x300.png)