Causes and risk factors
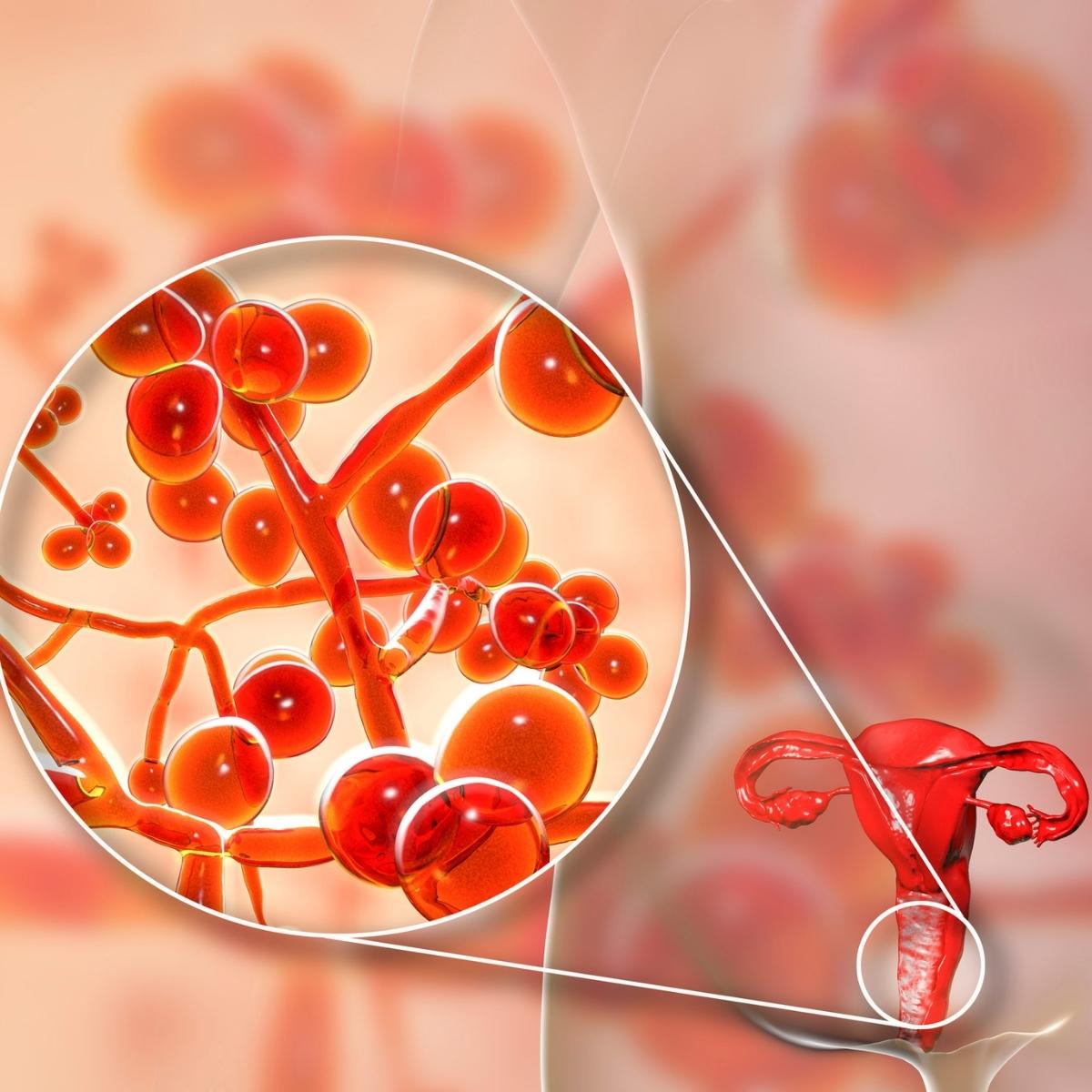
Vulvovaginitis is the commonest gynecologic problem of childhood. Prepubertally, the vulva, vestibule, and vagina are anatomically and histologically susceptible to infection with the bacteria typically present in the perianal area. The physical proximity of the vagina and vestibule to the anus results in overgrowth of bacteria that can cause primary vulvitis and secondary vaginitis. In prepubertal girls, vulvovaginitis is usually caused by multiple organisms that are present in the perineal area, although a single organism such as Streptococcus or rarely, Shigella, may be causative. Candidiasis, trichomoniasis, are additional causative factors for vulvovaginitis in adult females. Other causes of vulvovaginitis include yeasts, viruses, and parasites. Due to the acid base imbalance in the vaginal walls, there is overgrowth of organisms. Additional causes such as bubble bath, soaps, feminine perfumes, sprays, vaginal birth control methods. as well as vaginal insertions like tampons, ski skin diseases, . tight Tight-fitting, and nonabsorbent garments can lead to infection and thus vulvovaginitis. Menopause may be one of the causes of vulvovaginitis. Lack of cleanliness and personal hygiene can predispose to vulvovaginitis. Sexual abuse is one of the suspecting suspected causes for recurrent vulvovaginitis.
Clinical presentation
Patient presents with irritation and intense itching of the external genitalia. Patient experiences discomfort and burning while micturition. Inflammation of vagina and surrounding area is seen. There is foul foul-smelling vaginal discharge. There is brownish green discharge and irritation of labia and vaginal opening. Due to irritation and inflammation, the affected area becomes swollen red and rash develops.
Investigation
Medical history by the patient and clinical examination by the gynecologist helps in diagnosis. A wet prep examination is done to identify yeast infection. Routine heamogram and blood culture may be advised. Culture of vaginal discharge is recommended. Vaginal tissue biopsy confirms the diagnosis.
Treatment
Treatment depends upon the underlying cause. Yeast infections are treated by medicated creams and suppositories. Medicines like antibiotics, topical antibiotic creams may be required in case of Trichomonas or Chlamydia infections. Corticosteroids may be helpful. Antihistaminics Antihistamines may be required for controlling itching. Antifungal creams may be applied which will also help in managing vulvovaginitis. Cold compress contributes further to the treatment. Personal hygiene, loose garments will help in treating the condition further.
Other Modes of treatment
The other modes of treatment can also be effective in treating vulvovaginitis. Homoeopathy is a science which deals with individualization and considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly, the Ayurvedic system of medicine which uses herbal medicines and synthetic derivates are is also found to be effective in treating vulvovaginitis.