Causes and risk factors
Colonisation of spores of bacteria clostridium botulinum, through an open wound, boil, or abscess lead to wound botulism. Ingested bacteria release a neurotoxin in the intestine which is absorbed in the bloodstream. The toxin reaches neuromuscular junction causing symptoms of paralysis. It is seen in long term intravenous drug users [IDU] who are in their 50s or 60s, and who are on intravenous injections since many years.
Clinical presentation
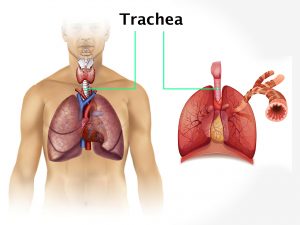
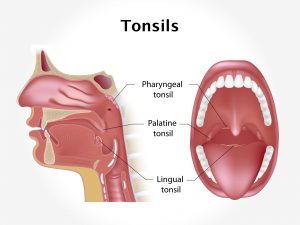
It presents with symptoms similar to botulism i.e. symmetrical cranial nerve palsy. Weakness of muscles of eye causing drooping of eyelids, double vision, weakness of muscles for chewing and swallowing, facial muscles causing slurred speech, dry mouth and throat, postural hypotension, constipation due to decreased peristalsis are some of the presenting features of botulism. Weakness then may spread to arms and legs. In severe cases paralysis of muscles of respiration causing dyspnoea, respiratory failure.
Investigation
Medical history by the patient and Clinical examination by the doctor helps in diagnosis. Diagnosis is done by identifying the bacterial toxin in food, stomach, intestinal contents, vomit or faeces.
Treatment
Treatment is done with antitoxin [human botulinum immunoglobulin], gastric lavage or enema if contaminated food is still present in gastrointestinal tract, ventilator support in case of respiratory failure. Paralysis recovers gradually.
Other Modes of treatment
The other modes of treatment can also be effective in treating paralysis caused by botulism.
Homoeopathy is a science which deals with individualization considers a person in a holistic way. This science can be helpful in combating the symptoms. Similarly the ayurvedic system of medicine which uses herbal medicines and synthetic derivates are also found to be effective in treating botulism.
Recent updates
Antitoxins are available for the known seven toxins produced by clostridium botulinum until now but Scientists have discovered new toxin called botulinum neurotoxin type H or BoNT/H, antitoxin for which is not yet available.