During the second wave of the Coronavirus, black fungus is primarily seen in many places of Nepal and many other nations worldwide. In Kathmandu and Kailali many cases have been discovered and soon reports the first death from Black fungus.
Black fugus is not a contagious disease, and it cannot spread from one person to another. It is most likely to impact those who have already suffered and weakened immune systems. And it’s a common occurrence with COVID-19 sufferers.
Causative and risk factor
Mucormycetes are a fungal infection-causing mold. Molds can be found in various environments, such as soil, air, and food.
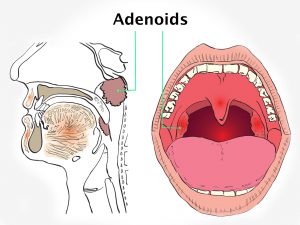
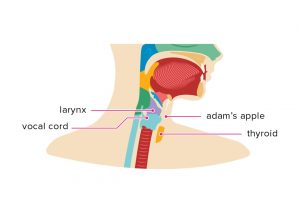
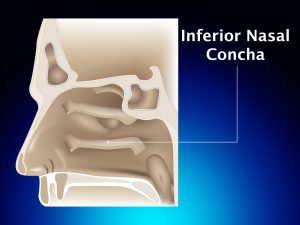
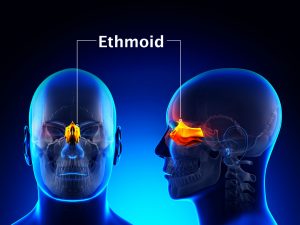
They enter the body through the nose, mouth, or eyes, and if left untreated, quickly they can cause brain damage.
The leading cause of black fungus (mucormycosis), according to medical specialists, is steroid usage during COVID treatment.
People with health disorders or who use medications that decrease their body’s ability to fight microorganisms and sickness are more prone to have black fungus (mucormycosis).
The main risk factor of black fungus is low immunity power, and the following are the peoples who are likely to get affected :
- Diabetic ketoacidosis, uncontrolled diabetes, and people with diabetes on steroids or tocilizumab are all risks.
- Patients on immunosuppressants or anticancer treatment and those with chronic debilitating conditions are at risk.
- Patients who have been taking large doses of steroids or tocilizumab for a long time
- COVID-19 Severity Cases, Patients who needed nasal prongs, a mask, or ventilatory support while on oxygen
Clinical presentation
- History and Physical Examination
Mucormycosis is categorized into six types based on anatomic location:
- Rhinocerebral
- Pulmonary
- Cutaneous
- Gastrointestinal
- Diffuse
- Unusual presentations.
Mucormycosis symptoms vary depending on the site of infection.
Symptoms:
Rhinocerebral disease
- Unilateral retro-orbital headache
- Facial pain
- Numbness
- Fever
- Hyposmia
- Nasal congestion with black discharge
Pulmonary disease
- Fever
- Dyspnea
- Cough
Cutaneous disease
- Discoloured skin patches (abnormal pigmentation)
- Dry skin
- Open sores, lesions, or ulcers
- Peeling skin
- Rashes, possibly with itchiness or pain
- Red, white or pus-filled bumps
- Scaly or rough skin
Gastrointestinal
Vague including stomach discomfort
Distention
Nausea and vomiting
Some patients experience palpable pain or a mass
Disseminated disease
Other diffused types of mucormycosis can affect the kidneys, bones, heart, and other organ systems, resulting in symptoms attributed to these organ systems.
Other forms include the central nervous system
Headaches, a decreased state of consciousness, and focal neurologic symptoms/signs, such as cranial nerve impairments, are all indicators of central nervous system disorders. Open head trauma, intravenous drug usage, or cancer are all possible causes of CNS involvement.
Investigation
People get infected by fungus spores that float around in the environment. The fungus can also be caught when it “enters the skin through a cut, burn, or other kinds of skin damage.”
When the fungus comes into contact with a bodily part, it might attach to it and proceed interior through the nose, sinuses, or lungs.
According to reports from several leading hospitals , patients suffer “blurred vision, darkening or blackening of tissue on the nose and cheeks, and black lesions within the mouth or drainage from the nose.”
According to current data, if a patient goes untreated or remains untreated for an extended period, their mortality rate can reach 80%. It’s still 40-50 percent if it’s addressed. Patients caught in the early stages of a sinus infection usually recover completely.
Scientists have developed a procedure to checkup for black fungus. A sample of the fluid from your nose is taken and sent to a lab for testing to determine if you have black fungus. To diagnose mucormycosis, the doctor may request a tissue sample, an MRI, or a CT scan.
And there are no blood tests available to detect Black Fungus.
Treatment
Antifungal medicine is often regarded as the most appropriate and successful therapy option. However, because the treatment duration can be extended to 8 months, the treatment plan is quite expensive. Amphotericin B is one of the most often utilized drugs, and the treatment period varies from 5 to 12 weeks until the patient recovers.
In certain severe cases, the treatment plan may require the removal of the damaged parts to prevent the fungus from spreading and keep the patient healthy. The FDA has just approved isavuconazole for use as a therapy.
Furthermore, studies have demonstrated the capacity of hyperbaric oxygen to cure black fungus since high-pressure oxygen can improve neutrophil efficiency in terms of fungal elimination.
Recent updates
The increasing number of cases of COVID-19 is assumed to be responsible for the rise in black fungus infections.
In Egypt, an 84-year-old patient with the black fungus was recently found to have been infected with the dangerous COVID-19 virus. Severe knee aches and an inability to stand on his feet were symptoms. On the other hand, the viral illness was treated without the patient suffering from kidney and lung failure.
The black fungus also infected his right eye, and the patient described his experience as one of the most terrible diseases that humans have ever faced.